International patients please learn more here or call 1.713.441.2340.
Radiation Therapy Treatments We Offer
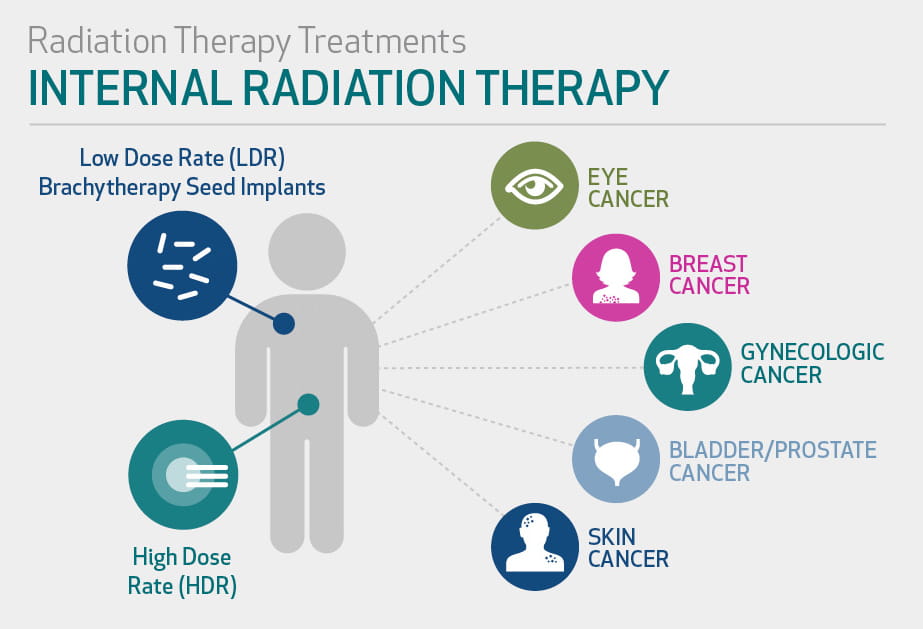
Depending on your specific type of cancer, your radiation oncologist may recommend either internal radiation therapy or external radiation therapy.
Internal Radiation Therapy
Internal radiation therapy is sometimes called brachytherapy. It may be used to treat:
During this type of radiation therapy, radioactive materials (isotopes) sealed in tiny pellets are placed in the tumor using devices, including needles or catheters. The isotopes give off radiation as they decay, which damages nearby cancer cells.
As an alternative method for treating some types of breast cancer, partial breast irradiation uses a catheter to deliver radiation to the tumor site and lumpectomy cavity.
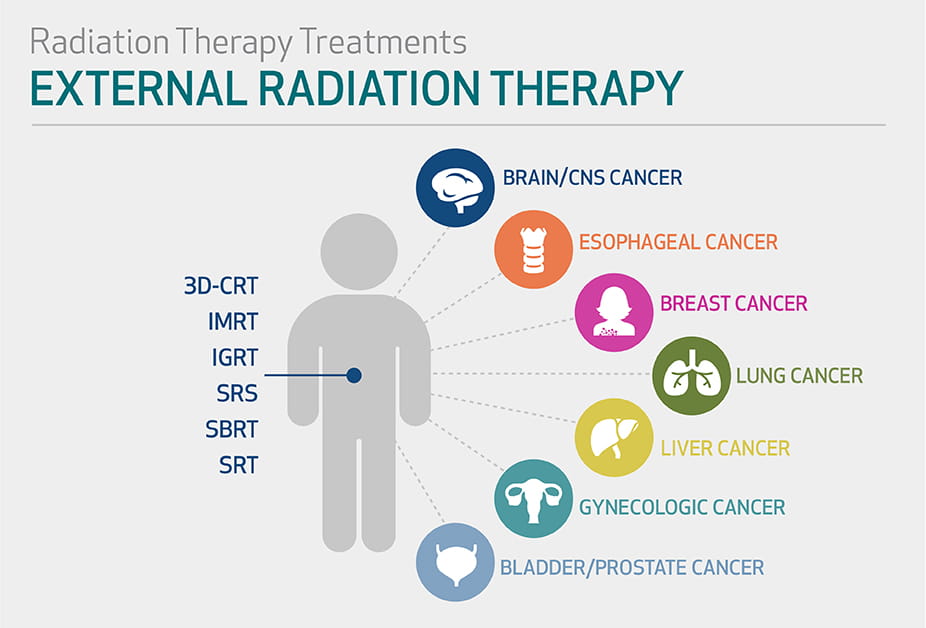
External Radiation Therapy
External radiation therapy uses external beams to damage cancer cells. It may be used to treat:
- Brain cancer
- Esophageal cancer
- Breast cancer
- Head and neck cancers
- Lung cancer
- Liver cancer
- Gynecologic cancers
- Bladder cancer
- Prostate cancer
There are several different types of external radiation therapy.
Types of External Beam Radiation Therapy
Radiation Therapy Technologies Our Experts Use
- TrueBeam – delivers powerful, accurate and fast image-guided treatments
- Novalis – an image-guided system that precisely forms a radiation beam around a tumor while protecting the healthy tissue
- TomoTherapy – confirms a patient's tumor before treatment and precisely delivers radiation therapy
- Varian Clinac 21EX – provides accurate, full-dose ranges for intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT)
- Phillips CT Simulator – provides precise and flexible scanning and dosing delivery
- Varian High Dose Rate (HDR) Afterloader – includes a computer-based management system allowing for proper placement, replacement and dosing