- Home
- ...
- Conditions & Treatments
- Heart Failure
- Hypertrophic Cardiomyopathy (HCM)
- Home
- Services & Specialties
- Heart and Vascular
- Conditions & Treatments
- Heart Failure
- Hypertrophic Cardiomyopathy (HCM)

Expert Treatment for Hypertrophic Cardiomyopathy
Expert Treatment for Hypertrophic Cardiomyopathy
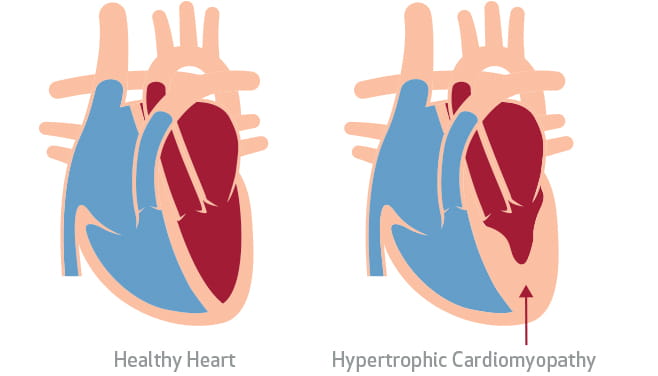
Hypertrophic Cardiomyopathy (HCM)
Hypertrophic cardiomyopathy (HCM) is a genetic heart disorder that can cause the muscle in your heart to thicken, making it harder for your heart to pump blood. Our HCM specialists are experts in diagnosing and treating hypertrophic cardiomyopathy, which can often go undetected until the condition advances to the point of becoming deadly.
Our Approach to Treating Hypertrophic Cardiomyopathy (HCM)
At Houston Methodist, our hypertrophic cardiomyopathy experts work as a team to provide a thorough evaluation and develop the most effective treatment plan for your specific condition. The team also works with you to help you make decisions best suited to your unique lifestyle needs.
Our specialists are experts in the nonsurgical and surgical techniques required to treat HCM, and cardiologists throughout the U.S. Gulf Coast refer patients to our team because of this expertise.

A Program Dedicated to Treating HCM
Specialists within the Houston Methodist Hypertrophic Cardiomyopathy Program are world-renowned experts in both diagnosing and treating HCM. Our program is recognized for our excellence by the Hypertrophic Cardiomyopathy Association (HCMA), the only one of its kind in Houston.
Choose a Doctor at One of Our Locations
Hypertrophic Cardiomyopathy FAQs
Hypertrophic cardiomyopathy (HCM) is a condition in which the normal alignment of the muscle cells in your heart is disrupted, creating irregular and disorganized structures. As a result, your heart muscle becomes thickened, especially in its middle section, where the right and left chambers are separated. If your septum becomes too thickened, it can block the outflow of the blood from the heart to the rest of the body.
HCM occurs when you inherit one of several possible gene abnormalities (mutations). You only need one copy of the abnormal gene to have this condition.
“If you have one of the abnormal genes that leads to HCM, you can begin to have symptoms as young as 10 years old — but most people manifest the disease later in life.
The heart usually thickens during puberty.
Symptoms of hypertrophic cardiomyopathy (HCM) may vary and can be mild or severe, but some or all of the symptoms are common, including:
- Shortness of breath, with or without exercise
- Chest pain
- Decreased tolerance to exercise
- Skipping, fluttering or racing of the heart (palpitations)
- Dizziness, lightheadedness or feeling like you might pass out, which may increase with activity
If you have HCM, you may be diagnosed at a young age or not until many years later. This is because the symptoms of HCM can mimic the symptoms of other more common conditions, such as:
- Asthma
- Being out of shape
- Anxiety or panic attacks
- Mitral valve prolapse (a common defect of the mitral valve leaflets)
The signs and symptoms of HCM can be so vague or unnoticeable that sudden death may be the only apparent indication of its presence — especially among young people.
If your doctor suspects you have hypertrophic cardiomyopathy (HCM), he or she will ask questions about your own medical history and your family’s medical history, such as whether or not:
- You have had shortness of breath or chest pain that worsens during exercise
- Anyone in your family has died at an early age from an unknown condition
- Anyone in your family has been diagnosed with HCM
An HCM specialist will also conduct a physical exam that includes:
- Checking your pulse, looking for a forceful or jerking pulse
- Looking and feeling for a rise in the left side of your chest with your heartbeat (a heave)
- Listening for a heart murmur or irregular heartbeat with the stethoscope
- Checking your blood pressure while you're lying sitting, standing and after a quick brisk walk
Your doctor may also use a blood test to perform genetic testing. The test may show which gene abnormality is causing HCM in your case. Your family members can then be screened looking for that particular gene.
Most of the diagnostic tests used to diagnose HCM are noninvasive and include:
- Electrocardiogram (ECG/EKG) – to check for changes indicating your heart is enlarged (left ventricular hypertrophy) and for an arrhythmia
- Echocardiogram – an ultrasound of the heart that shows how well your heart pumps, how thick the muscle is, the function of your heart valves, and if there is any turbulence of blood flow as it leaves the heart
- Holter monitor – worn for 48 hours to 30 days to check for electrical instability (arrhythmias)
- Cardiac stress test – measures your heart function under stress (exercise), usually done on the treadmill and often performed while wearing a mask during the test to measure how much oxygen you are using
- Cardiac MRI – uses magnetic fields and radio waves to measure thickness of your heart muscle, how well the walls of the chambers of your heart move, how well your heart's valves are working, as well as if there is obstruction of the blood going out of your heart to the rest of your body
- Cardiac catheterization – a catheter-based procedure that shows your coronary arteries and the pressure in your heart — however, this test is not often used when diagnosing HCM
Depending on the severity of your condition, treatment for hypertrophic cardiomyopathy (HCM) can include lifestyle modifications, medications, nonsurgical alcohol septal ablation and surgical myomectomy.
In addition, an implantable cardioverter-defibrillator (ICD) may be recommended if you have any life-threatening arrhythmias such as ventricular tachycardia or ventricular fibrillation, or if you have risk factors for such arrhythmias.
Lifestyle Modifications for HCM
To help reduce complications and make you feel better mentally and physically, the following lifestyle modifications are recommended:
- Get regular exercise (low intensity and avoiding strenuous physical activity)
- Avoid competitive sports
- Maintain a healthy diet
Medications for HCM
There are several medications that can help reduce your symptoms and restore your heart to its normal function, including:
- Beta blockers – can help control irregular heartbeats and decrease obstruction to blood flow in your heart
- Calcium channel blockers – help your heart beat slower and decrease obstruction to blood flow in your heart
- Antiarrhythmia medications – help control your heart’s rhythm
- Blood thinners – help prevent blood clots that can form as the result of an arrhythmia
Nonsurgical Alcohol Septal Ablation for HCM
Alcohol septal ablation is used to thin the thickened part of your heart muscle to help improve blood flow. During this procedure, a small portion of the thickened heart muscle is injected with alcohol using a catheter.
A complication of this treatment can be heart block, where your heart’s electrical system is affected such that you may require a pacemaker to be implanted to help your heart beat at a normal rate.
Surgical Myomectomy for HCM
A myomectomy is an open-heart surgical procedure that may be recommended if medications do not relieve your HCM symptoms. After this procedure, most people no longer experience HCM symptoms.
During this procedure, the surgeon removes part of the thickened muscle in the septum between your heart's ventricles. This removes the obstruction of blood flow caused by the thickened muscle, improving blood flow to the body.
Implantable Cardioverter-Defibrillator (ICD) for HCM
If you have any life-threatening arrhythmias, such as ventricular tachycardia or ventricular fibrillation, or risk factors for these arrhythmias, your care team may recommend an implantable cardioverter-defibrillator (ICD).
An ICD is a small device implanted under your skin (near your collar bone) that continuously monitors your heart for life-threatening arrhythmias. A specialized team of electrophysiologists will implant the device and monitor it on a regular basis.
If a dangerous rhythm is detected, your ICD will attempt to pace you out of the dangerous rhythm. If that is unsuccessful, your ICD will deliver a shock to terminate the dangerous rhythm and prevents sudden cardiac death (SCD).
