Professional Contributions of Nursing at Houston Methodist Hospital
Houston Methodist Hospital nurses use the Magnet® Model as a framework for nursing excellence. Through Transformational Leadership, Structural Empowerment, Exemplary Professional Practice, and New Knowledge, Innovation and Improvements, excellent empirical outcomes are achieved. Houston Methodist Hospital nursing supports the Houston Methodist vision for unparalleled safety, quality, service and innovation.
Nursing mission: Houston Methodist nursing provides an environment in which excellent nursing practice, interprofessional collaboration, leadership, education and research ensure that patients, families and the community experience compassionate, value-based care through unparalleled safety, quality, service and innovation.
Nursing vision: We lead the world of nursing in an innovative and collaborative environment of excellence in patient care, education and research.
Philosophy of nursing: We believe the cornerstone of the Houston Methodist Professional Practice Model is a triad of:
- Leadership: Building value-driven partnerships with patients, families and the interprofessional team that yield high-quality care.
- Art: Caring for patients and families in a holistic way to meet clinical, psychological, educational and spiritual needs.
- Science: Improving outcomes through evidence-based practices, research, innovation and professional development.
Transformational Leadership
Nurse leaders and nurses at the bedside are transformational leaders who keep nursing goals aligned with the vision and mission of the hospital. They participate in leadership development and mentorship programs, and demonstrate advocacy and support on behalf of staff and patients.
Structural Empowerment of Nursing
Shared Governance — A Model for Nursing Leadership
Nurses at Houston Methodist Hospital are empowered to share experience and knowledge by participating in collective decision-making with interprofessional colleagues. Shared Governance is a decision-making model that offers clinicians the means to influence professional practice and the quality of patient care, as well as to build leadership skills. Shared Governance supports the strategic goals of nursing, thus providing better care to our patients and families.
Houston Methodist Shared Governance Model

Recognition for Contributions to Professional Nursing
- Nurses at Houston Methodist Hospital are routinely recognized for professional accomplishments throughout the year by receiving the following awards:
- Daisy Award
- Annual Brown Foundation Outstanding Nurse Clinician Award (1st place: $15,000, 2nd place: $2,500, 3rd place: $1,000)
- Annual Early Career Nurse Award
- Good Samaritan Foundation Nurse Excellence Award
- Houston Chronicle Salute to Nurses
- Texas Nurses Association District 9 Nurse Excellence Award
- Annual Nursing Excellence Award
- ICARE Award
- Nurse Team Spirit Award
- Houston Methodist Hospital recognizes nurses for dissemination of research and evidence-based practice by providing resources to:
- Attend conferences to present our findings to national and international health care professionals
- Publish articles in professional journals
- Nurses are recognized to volunteer locally, nationally or internationally by providing paid time off (ICARE in Action) and additional resources (supplies/educational material/donation).
- Nurses are recognized by the organization for professional development and are encouraged to be life-long learners by providing:
- Tuition assistance of $4000 a year
- Voucher Programs for Nursing Certifications
- Graduate Nurse Residency Program
- Clinical Scholar Program for evidence-based practice and research
- Shared Governance Leadership Series for Shared Governance front-line leaders
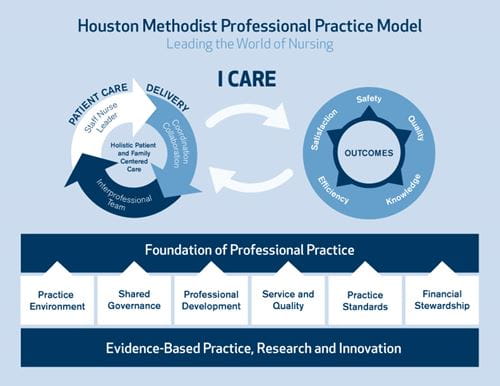
Houston Methodist Professional Practice Model
Exemplary Professional Practice
Houston Methodist’s I CARE values of integrity, compassion, accountability, respect and excellence provide the overarching values that guide service and practice. The Houston Methodist Professional Practice Model describes the patient care delivery system and the practice of professional nursing.
The patient care delivery system keeps the patient and family at the center, with the staff nurse leader in communication and collaboration with the interprofessional team to affect outcomes of safety, quality, knowledge, efficiency and satisfaction. The graphic depiction above shows our Professional Practice Model, which is built upon evidence-based practice, research and innovation.
New Knowledge, Innovations and Improvements
Houston Methodist Hospital Nursing Publications
-
Del Pino, M, Rivero, P, Taylor, A, Gabriel, R. (2025), Impact of Depression and Cardiovascular Risk Factors on Cognitive Impairment in Patients with Atrial Fibrillation: A Systematic Review and Meta-Analysis, Archives of Gerontology and Geriatrics, 128. https://doi.org/10.1016/j.archger.2024.105601
-
Guerrero, K, Fleming, S, Calderon, A and Fontenot, N (2024), Original Research: Addressing Nurse Burnout: The Relationship Between Burnout and Physical Activity, AJN 124(6): 20-26. https://doi.org/10.1097/01.naj.0001023020.53993.34
-
Ortiz Carter, L, Carter, G, Fielden, A (2024), Just in Time: Improving Preoperative Checklist Compliance in the Cardiac Cath Lab, Journal of PeriAnesthesia Nursing, 39(4):e29-e30. https://doi.org/10.1016/j.jopan.2024.06.075
-
Paredes, C, Reed, K, Moore, L, Brant, JM. Perianal Injury Prevention in Patients with Leukemia. Clin J Oncol Nurs. 2024 Mar 15;28(2):149-156. https://doi.org/10.1188/24.cjon.149-156
-
Loewy, S, Jelks, A, Greene, T, Vozzella, G, Fontenot, N, & Muyco, J. (2024). Optimizing Delegation to Maximize Nurses’ Time: Results of a Time Study in an Acute Care Setting. Journal of Nursing Education and Practice. https://doi.org/10.5430/jnep.v14n6p43
-
Knippa, S, Coakley, S. & Hehman, M (2024). History and Professional Legacy of Nursing Certification, Critical Care Nurse, 44(1): 67-72.
-
Sheen, L. H., Casarez, R., Gallagher, M. R., Hayes, A.E., Diep, C. S., & Engebretson, J. (2024). Understanding Diabetes Self-Management Among Vietnamese Americans: A Focused Ethnography. Journal of Transcultural Nursing, 35(2), 142–150. https://doi.org/10.1177/10436596231217698
-
Schwartz, R. L., Hamlin, S. K., Vozzella, G. M., Randle, L. N., Klahn, S., Maris, G. J., & Waterman, A. D. (2024). Utilizing Telenursing to Supplement Acute Care Nursing in an Era of Workforce Shortages: A Feasibility Pilot. CIN: Computers, Informatics, Nursing, 42(2), 151-157.
-
Broadway, K., & Nuila, C. M. (2023). Implementation of an Interprofessional Mobility Program in a Neurosurgical Intensive Care Unit. Journal of Neuroscience Nursing, 55(6), 205-210.
-
Hamlin, S. K., Fontenot, N. M., Hooker, S. J., & Chen, H. M. (2023). Systems-Based Physical Assessments: Earlier Detection of Clinical Deterioration and Reduced Mortality. American Journal of Critical Care, 32(5), 329-337.
-
Hamlin, S., Fontenot, N. and Chen, HM. (2023). Rapid response teams and code management. Introduction to Critical Care Nursing, 9th ed. St. Louis: Elsevier.
-
Hayes, AE, Wardell, DW., Engebretson, J., LoBiondo-Wood, G., & Allicock, M. (2023). Psychosexual responses to BRCA gene mutations in women of childbearing age. Journal of the American Association of Nurse Practitioners, 35(4), 242-251.
-
Hehman, M. (2023). “Give Equal Prominence to the Role of the Nurse”: Power, Partnerships, and the Role of Expert Nursing in Premature Infant Care in the United States, 1922-1943, Nursing History Review, 31(1): 93-126.
-
Hehman, M.C. (2023) Introduction: Special Section, Nursing in Wartime, Nursing History Review, 31(1): 31-34.
-
Hehman, M. C., Fontenot, N. M., Drake, G. K., & Musgrove, R. S. (2023). Leveraging digital technology in nursing. Health Emergency and Disaster Nursing, 10(1), 41-45.
-
Moore, L., & Alexis Elizabeth Hayes. (2023). Cancer Health Literacy in Black Women With Breast Cancer: A Comprehensive Literature Review. Clinical Journal of Oncology Nursing, 27(5). https://doi.org/10.1188/23.cjon.507-513
-
Quintero-Pena, C., Qian, P., Fontenot, N. M., Chen, H. M., Hamlin, S. K., Kavraki, L. E., & Unhelkar, V. (2023, August). Robotic Tutors for Nurse Training: Opportunities for HRI Researchers. In 2023 32nd IEEE International Conference on Robot and Human Interactive Communication (RO-MAN) (pp. 220-225). IEEE.
-
Vozzella, G. M., & Hehman, M. C. (2023). Cardiovascular Nursing Workforce Challenges: Transforming the Model of Care for the Future. Methodist DeBakey Cardiovascular Journal, 19(2), 90.
-
Fontenot, N. M., Hamlin, S. K., Hooker, S. J., Vazquez, T., & Chen, H. M. (2022, July). Physical assessment competencies for nurses: A quality improvement initiative. In Nursing Forum (Vol. 57, No. 4, pp. 710-716).
-
Hamlin, S., Fontenot, N., Chen, H. M., & Hooker, S. (2022). 1231: Nursing Assessment Reduces Delays In Rapid Response Team Activation, ICU Admissions, And Mortality. Critical Care Medicine, 50(1), 616.
-
Hehman, M. C. (2022). Nursing Care of Refugee Children: A Historical Perspective. Pediatric Nursing, 48(5), 215-221.
-
Hehman, M.C. (2022). Nursing Care of Refugee Children: A Historical Perspective, Pediatric Nursing, 48(5): 215-221.
-
Hehman, M.C. (2022) Introduction: Special Section, Past as Prologue—The 1918 Influenza Pandemic and COVID-19: Introduction, Nursing History Review, 30(1): 9-13.
-
Macapagal, F. R., Bonuel, R., Rodriguez, H., & Mcclellan, E. (2021). Experiences of patients using a fitness tracker to promote ambulation before a heart transplant. Critical Care Nurse, 41(4), e19-e27.
-
Branson, S., Boss, L., Hamlin, S., & Padhye, N. S. (2020). Animal-assisted activity in critically ill older adults: a randomized pilot and feasibility trial. Biological Research for Nursing, 22(3), 412-417.
-
Hamlin, S., Fontenot, N., & Chen, H. (2020). Innovative nurse-driven solutions to complex patient issues: Methodist proficiency assessment and competency certification. American Journal of Medical Quality, 35(IS), 29S.Ramundo, J., Coverstone, S., Crumbley, D. R., Geiger, D., Jankowski, I., Ritter, D., ... & Wound Treatment Associate Advisory Committee. (2020). Evaluation of the Impact of the wound treatment associate (WTA) education program on practice and quality patient outcomes. Journal of Wound Ostomy & Continence Nursing, 47(1), 13-19.
Scholarly Contributions of Nursing — Poster and Podium Presentations
-
Hehman, M.C., Hayes, A.E, & Muyco, J.D. (May 2024) “Meaningful Recognition for Nurses: Contemporary Practices for a Diverse Workforce,” podium presentation at the American Association of Critical Care Nurses NTI 2024 Conference, Denver, CO.Fontenot, NM., Ramos, C. & Dubose, T. March 2024. “Perception vs. Reality: Assessing the Health of Shared Governance.” Podium Presentation. Sigma’s Creating Healthy Work Environments Conference. Washington, D.C.
-
Hehman, M., Fontenot, NM & Ramos, C. March 2024. “Creating Healthy Work Environments to Support, Retain, and Grow the Next Generation of Nurses.” Podium Presentation. Sigma’s Creating Healthy Work Environments Conference. Washington, D.C.
-
Senneff, J., Ramos, C., Hehman, M., & Fontenot, N.. March 2024. "Supplementing the Nurse Residency Program to Support, Retain, and Grow the Next Generation of Nurses. Poster Presentation. Vizient AACN/NRP Annual Conference. San Diego. CA.
-
Hehman, M.C. (September 2023) “The Nurses of Ellis Island: The Power of Place,” podium presentation at the 40th Annual American Association for the History of Nursing Conference, Pittsburg, PA.
-
Hehman, M.C. (July 2023) “The Nurses of Ellis Island: Policy and Place,” virtual podium presentation at the Sigma 34th Annual International Nursing Research Congress, Abu Dhabi, United Arab Emirates.
-
Hehman, M.C. (May 2023) “Past as Prologue: The Role of History in Nursing Education and Practice,” podium presentation at the American Association of Critical Care Nurses NTI 2023 Conference, Philadelphia, PA.
-
Sosa, L., Muyco, J., Asirifi, K., Roy, S., Freeman, M., & Johnson, B. (2023, July). Utilizing a Nursing Team Handoff to Improve Communication, Teamwork, and Perception of Care and Safety. In Sigma's 34th International Nursing Research Congress. Sigma.
-
Quintero-Pena, C., Qian, P., Fontenot, NM., Chen, HM, Hamlin, SK., Kavraki, L., & Unhelkar, V. August 2023. “Robotic tutors for nurse training: Opportunities for HRI researchers.” Podium Presentation. Institute of Electrical and Electronic Engineers’ RO-MAN 2023. Busan, Korea.
-
Ramos, C. D. (2023, August). The Impact of Electronic Health Record Data Fields on Patient Outcomes. In Sigma's 34th International Nursing Research Congress. Sigma.
-
Carter, L. O., & Fielden, A. (2023). Care of Obstetric Patients in the Postanesthesia Care Unit. Journal of Obstetric, Gynecologic & Neonatal Nursing, 52(4), S36.
-
Fontenot, NM., Lauw, C., Gathogo, K., Lemeshev, R., & Asirifi, K. July 2023. “Student Nurse Scribes: A Unique Pilot to Reduce Nurses’ Documentation Burden. Poster Presentation. Sigma’s 34th International Nursing Research Congress. Abu Dhabi, EAU.
-
S. Hamlin, N.M. Fontenot, & M. Chen, January 2022. “Nursing Assessment Reduces Delays in Rapid Response Team Activation. Podium Presentation. 2022 Critical Care Congress. Virtual.
-
Chen, HM, Fontenot, NM, & Hamlin, S. July 2021. “A Systematic Physical Assessment Training Reduced Hospital Mortality Rate.” Podium Presentation. Sigma’s 32nd International Nursing Research Congress. Virtual.
-
Leaders, T., Ortiz-Carter, L., & Fielden, A. (2021). Oh Baby! There's a Pregger in My PACU…. Journal of PeriAnesthesia Nursing, 36(4), e1.
-
Macapagal, F. R., Rodriguez, H. M., Bonuel, R. M., & McClellan, E. G. (2020). Use of common technology (Fitbit) as an aid to increase ambulation among pre-heart transplant patients.
