Kenneth R. Peak Brain & Pituitary Treatment Center Research Projects
The Targeted Cancer Treatment laboratory is the heart of the Peak Center research activities. It identifies and develops novel targets and delivery mechanisms to kill brain tumors and unravels the mechanisms that make these treatments work. The work from this laboratory feeds into the many other labs in the Peak Center who further develop and refine these novel treatments. Projects include the development and refinement of Nano syringes that make individual injections into cancer cells, demonstration of the world’s first example of selective mitochondrial chemotherapy, and discovery of unique glucose transporters that exist in cancer cells only that can be utilized by novel molecules and poison the cancer cells’ energy supply. Additional work is underway relating to differences in immune privilege in male and female cancer cells, and the development of serum biomarkers to diagnose brain tumors and monitor the success of therapy.
PAM OBG: A first-generation monoamine oxidase B activated prodrug specifically targeting MGMT
Treatment of GBM using monotherapy fails due to various reasons, such as drug resistance, DNA repair pathway activations, levels of active MGMT in GBM to mention a few. Drug such as 06BG is an alkylating agent and a potent inhibitor of MGMT is nontoxic when administered as a single drug, but has shown to be toxic when co-administered with other alkylating agents in non-tumor tissues, especially bone marrow. Due to these reasons, Dr. Sharpe designed a prodrug, PAM-OBG as a monoamine oxidase B (MAOB) activated MGMT inhibitor. This prodrug based on MAOB activation gets converted into its active form only in GBM cells, as already published GBM cells express high levels of the enzyme MAOB.
In the laboratory, an early testing in an in vitro and in vivo environment was performed on this compound that was designed in-house by Dr. Sharpe and team. Outcomes of studies conducted in the laboratory was published in Oncotarget 2018.
Dr. Sharpe and team are currently synthesizing four prodrugs, which will be tested in an intracranial mouse model of GBM to be presented to FDA as a drug candidate. A GLP grade synthesis is under work for this compound for scale-up and future use, using combiflash. Dr. Sharpe and Dr. Baskin have received TRI Award for $1.3 million in funding to advance a MAOB prodrug into a Phase I clinical trial.

Houston Methodist: Mitochondria Based Chemotherapy – Patient from Houston Methodist on Vimeo.
MP-PT(IV) is a second-generation prodrug that is a MAOB prodrug that targets GBM mitochondria. This compound was synthesized in the laboratory by Dr. Sharpe and has been tested in vitro and in vivo. MP-PT(IV) combines the benefits of MAOB enzyme conversion into an active form as well as generation of cisplatin inside GBM cells causing targeted toxicity.
The efficacy of MP-PT(IV) was studied in vitro and in intracranial patient derived xenograft mouse model. This prodrug has also shown to potentiate existing standard of care therapy i.e. Temozolomide with radiation. A GLP grade synthesis is under work for this compound for scale-up and future use using combiflash for which Drs. Baskin and Sharpe have received TRI Award of 1.3 million by HMAI.

Epitope-targeted nanosyringes: peptidyl-coated nanovectors to bind to GBM cells receptors to create our drug-laden Trojan-horses
Nanosyringes are capable of delivering large amounts of drugs directly into the cancer cells with targeted surface epitopes. In the past, an antibody targeted as well as peptidyl targeted nanovector system was developed by Dr. Baskin and Dr. Sharpe. The two methods of delivering drugs in cancer cells were based on polyethylene glycosylated hydrophilic/hydrophobic carbon cluster (PEG-HCC) nanosyringes. These syringes can be filled with hydrophobic compounds such as chemotherapeutics and target them to cancer cells using antibody of peptides.
Many in vitro and in vivo studies performed in the laboratories demonstrated the specificity of this drug delivery system by killing only brain tumor cells and not normal human astrocytes and neurons. In addition to delivery of chemotherapeutic drugs, this delivery mechanism was also used to inject drug pump inhibitors to fight drug resistance developing in cancer cells.
Selected surface antigens on cancer cells are either not present or in very low levels in other body cells and therefore this mechanism gives an advantage of low off-site toxicity. This enables us to deliver higher concentrations of chemotherapy to cancer cells and no other tissues of the body, increasing the treatment efficacy with low toxicity.
This model has been tested successfully in in vitro and intracranial mouse models with patient derived xenograft. Following interactions with the FDA personnel and reviewers recommendations the HCC core of the nanovector has been replaced. The Second generation of peptidyl-targeted nanosyringes that have high flexibility, allowing the delivery of both hydrophilic or hydrophobic payloads, including, but not restricted to, drugs, proteins, peptides, DNA, RNA and almost any combination of these.
Novel Targets , Therapeutics & Drug Delivery Systems

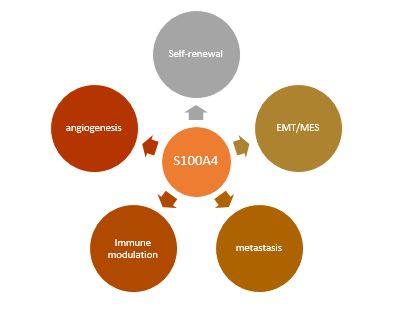
MOLECULAR MECHANISMS OF S100A4 FUNCTION IN GLIOMA STEM CELLS
CHARACTERIZATION OF BRAIN & PITUITARY TUMOR METABOLOMICS
Novel Brain Cancer Research
INVESTIGATIONS OF DYSREGULATED METABOLISM IN BRAIN & PITUITARY TUMORS


