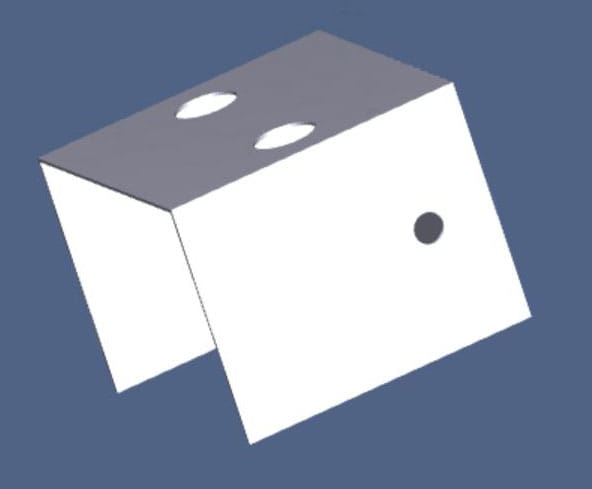
Isolation Box (V1)
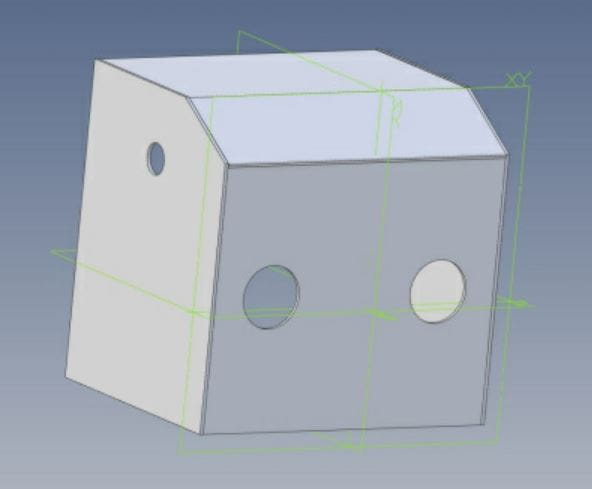
Short Slanted Isolation Box (v2)
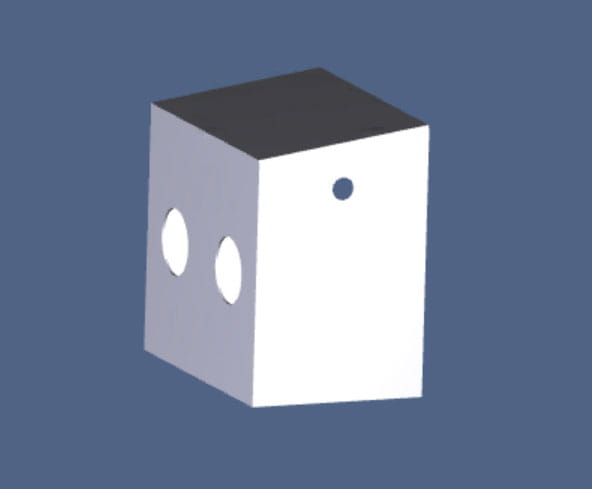
Houston Methodist Aerosol Container (V3)
ZIP of Individual Panel Specs
Download Houston Methodist Aerosol Container User Guide
Read more about the Aerosol Container and the Houston Methodist team behind it here.
Designs based on the Aerosol box design by Dr. Lai Hsien Yung.
Design specs for the Houston Methodist Aerosol Container include:
- 60cm tall, 60cm wide, 40cm in depth
- Two arm holes 15cm wide
- Front panel is 55cm with an 8-degree angle to create a slant to account for operator height
- Units fabricated from transparent polycarbonate boards
- Two side holes for vacuum device (see below): 12cm from top, 20cm from front, 5cm in diameter NOTE: This is for testing only, not for use with patients while in test phase.
- Sides glued together with #16 fast set acrylic cement
- Sides can be quickly and easily sterilized with 70% alcohol
- Recommend closing the side of the container facing away from the care provider to better contain aerosols by attaching a drape made with any sterile material and attached with tape

Vacuum Attachment for Negative Pressure
The next step for this prototype is adding a vacuum attachment to the HMAC through the side of the box to remove undesirable aerosol so that no particulate matter is left on the hands during intubation. NOTE: The vacuum attachment prototype is in test phase only and not for use with patients.
The vacuum used is the Atrix Omega Plus H14 ULPA (Ultra Low Penetration Air) vacuum. This is an immediate containment option for glove bag, abatement, and hazardous particulate applications. The ULPA vacuum specs include:
- A 1,000-hour rated Ametek® Advantek II motor
- 10’ detachable power cord
- One-gallon ULPA filter, 99.999% efficient at .12 micron with three layers of 56 pleat media
- the three layers consist of one cellulose layer and two glass layers
- Hose and filter plugs to contain debris during transport or storage
The vacuum attachment is in testing by Firas R. Zabaneh, MT(ASCP), CIC, CIE, MBA, Director of System Infection Prevention & Control - Houston Methodist System Quality & Patient Safety, at The Houston Methodist Institute for Technology, Innovation & Education (MITIESM), as seen in the video below.
Here the team simulates vomiting and hemoptysis as opposed to a forceful cough and continuous aerosol during intubation.
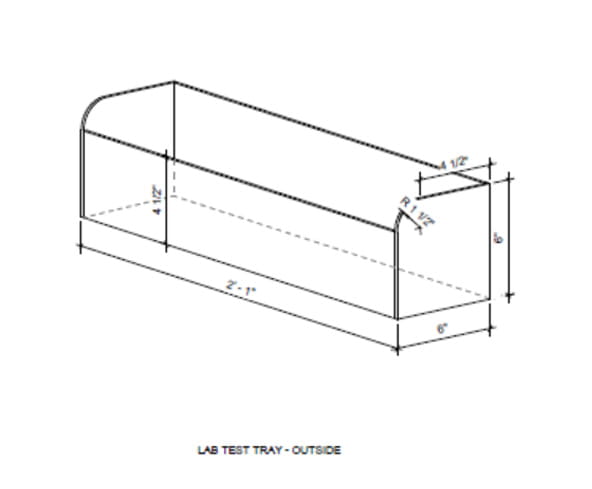
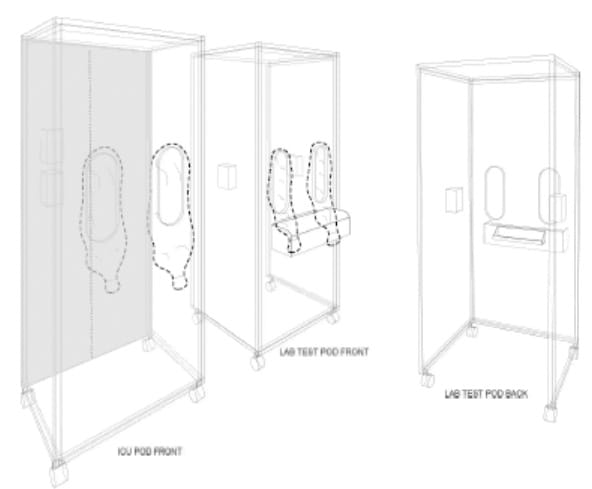
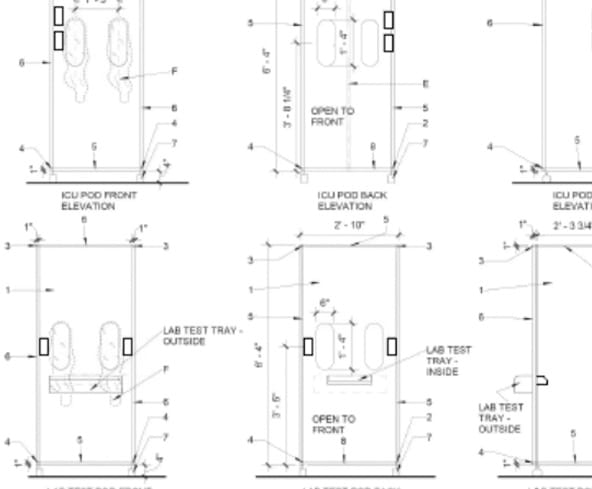
ICU Pod - Tray Views
ICU Pod - Isometric View
ICU Pod - Plan & Elevation View
The lab test pod is designed for health care workers who need to take a nasal draw to test patients for new coronavirus disease 2019. The patient may sit or stand in front of the pod, protecting the health care worker taking the sample so that the patient can tilt their head back and provide a good angle for the nasal swab during the procedure. The pod contains a small shelf with clean swabs and an external enclosed shelf area to drop the sample in a bag and allow for pick up outside the pod. Gloves are the only necessary PPE for use with the lab test pod.
The external surfaces of both pods must be wiped down with disinfectant after each use. The external surface of the pod sleeves should also be cleaned, but the internal surfaces of the sleeves and pod are intended to stay free of contamination. The health care worker must discard their gloves used during any patient procedure before pulling their arms back in the pod and immediately perform hand hygiene.
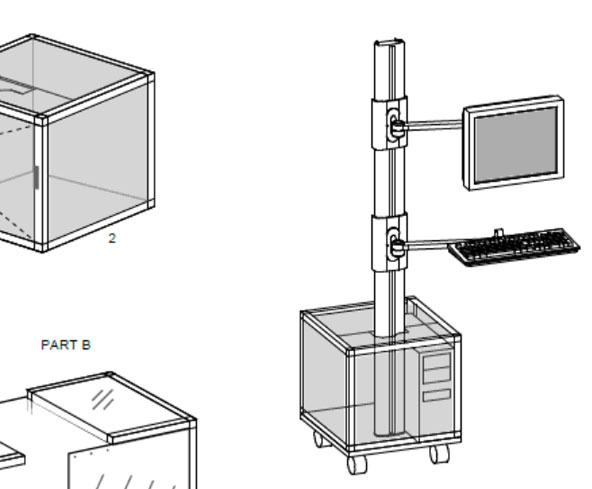
Bedside Monitor Containment Box
The Houston Methodist Neurophysiology team has developed an innovative design for a custom plexiglass box that prevents equipment contamination while working in COVID-19 patient isolation rooms. The computers they use are integrated on specially designed NATUS mobile carts. Each computer, installed at the bottom of each cart, is difficult to wipe down--only the outside of the computer can be disinfected. The plexiglass containment box surrounds the base of the cart, which then protects the computer, cables, WiFi bridge and other integrated equipment. The monitor, keyboard and all other equipment are wiped down separately. As an added benefit, there have been less equipment issues and failures noted by the staff since the install.
Solving the challenge was a collaborative effort. Neurophysiology team members Amy Reynolds and Robin Chong worked with Jens Larson, David Duncan and Larry McCarty in Facilities Maintenance Services to devise a prototype called the Bedside Monitor Containment Box. They tested the device for temperature control and obtained approval from both IT and Infection Control prior to implementation. The innovative box offers a huge leap forward in the ability to prevent equipment contamination in patient isolation rooms. . The team is sharing the prototype design for use systemwide.