Three-Year Uveal Melanoma Study Yields Extraordinary Results
Jan. 24, 2023 - Eden McCleskeyOf the 212 uveal melanoma patients treated with eye plaque brachytherapy at Houston Methodist over the past five years, a surprising number has gone on to experience local recurrence: zero.
All the patients achieved local control, according to a recent three-year outcomes study published in Journal of Contemporary Brachytherapy. The study also found distant metastasis and radiation-related toxicity rates were favorable compared to established norms.
"Because the study's local control rate at three years is better than any previously published rates, it is likely that we will see an improvement in long-term survival rates at 10 years, 15 years and beyond," says Dr. Amy Schefler, a Houston Methodist ocular oncologist and the study's principal investigator.
With the publication of these results, Houston Methodist becomes the U.S. center with the lowest rates of local recurrence for uveal melanoma.
Under the direction of Dr. Schefler and medical oncologist Dr. Eric Bernicker, the eye cancer team at Houston Methodist was already one of the highest profile and highest volume centers in the nation.
"As one of only a few hospitals in the country performing this advanced procedure, we target and destroy eye tumors while preserving vision — with virtually no chance of recurrence," says Dr. Schefler.
Practice makes perfect
Dr. Schefler attributes the team's success to a complex and highly personalized model of care, as well as years of specialized training and experience treating this rare disease.
"For every patient, we provide extensive presurgical planning with 3-D simulation software, custom-designed and custom-built ocular discs, personalized radiotherapy doses, intraoperative ultrasound guidance and cutting-edge biopsy techniques," Dr. Schefler explains. "Many centers do some of these things for some patients, but we believe you have to do all of them, consistently and frequently enough that it becomes routine, in order to begin moving the needle on outcomes."
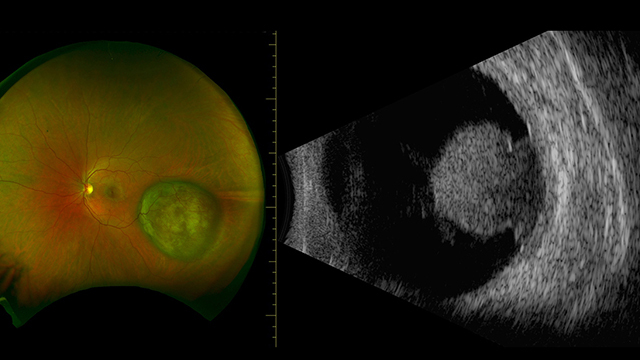
Uveal melanoma is the most common primary intraocular tumor in adults, forming in either the iris (4%), ciliary body (6%) or choroid (90%).
Although it only impacts a small number of people in the U.S. each year (about 2,500), it is considered the most severe form of eye cancer. An estimated 40%-50% of all diagnoses end in metastasis and eventually death within 20 years.
Local recurrence greatly increases the risk of metastasis.
Customized solutions for every tumor
Comprised of radiation oncologists, ocular oncologists, radiation physicists, ocular ultrasound technicians and eye pathologists, the eye cancer team at Houston Methodist uses an innovative brachytherapy approach to precisely deliver radiation to a patient's eye tumor using an implanted disc customized for the specific size, shape and contour of the tumor.
Dr. Bin Teh, a radiation oncologist, selects and designs radiation beads, known as seeds, for each patient based on eye tumor size, shape and configuration. The seeds are placed in a gold-backed, bottle cap-shaped implant that helps protect healthy surrounding tissue.
"Because everything is customized and built to spec, we are able to treat a wider range of tumors than those who rely on standard, commercially available options," Dr. Schefler says. "The ability to successfully treat smaller tumors impacts the positive long-term survival outcome in uveal melanoma, while the ability to treat larger, more aggressive tumors helps extend survival and improve quality of life for patients with the most advanced forms of the disease."
Fine-needle aspiration biopsies, performed for even the smallest and most difficult to sample tumors, provide critical information about the genetic expression profile of the tumor. This helps the care team determine the best course of treatment as well as whether there's a risk of the cancer spreading from the eye to other parts of the body.
"Our ocular pathologist, Dr. Patricia Chévez-Barrios, comes to the operating room for every case, looks at the sample and tells us right then and there if we got enough cells or need to go back and get more," Dr. Schefler says. "To my knowledge, we are the only program that does this. It adds a lot of value by greatly reducing the number of inconclusive biopsies."
Intraoperative ultrasound a key differentiator
The study's excellent local control rate — for lesions ranging across all sizes and genetic expression profile classes — emphasizes the importance of image-guided brachytherapy with intraoperative ultrasound.
Intraoperative image guidance is used to confirm the precise placement of the plaque and ensure adequate coverage of the tumor, providing a degree of accuracy beyond what traditional surgery can achieve.
"In about one out of every six cases, we can tell that we're slightly off the mark, so we immediately go back in and recenter the plaque on the tumor," Dr. Schefler says. "Real-time ultrasound guidance is what makes that possible. It is an important factor in minimizing treatment failure."
Unfortunately, only a few centers in the United States currently offer it to their patients.
"You have to have the right facilities and technology, yes, but the bigger issue is finding the right staff," Dr. Schefler says. "There are only a handful of these highly trained, highly skilled specialists — not enough to go around."
Dr. Schefler hopes this study — and its eye-catching results — will inspire more programs to invest in the resources and training necessary to put similar best practices in place.
"This is not an easy disease to treat, but it gets easier with each case," Dr. Schefler reflects. "It's rewarding to see the impact of your efforts in patients' lives and the small but steady uptick in survival rates."