What Is Monoclonal Antibody Therapy & Who Is Eligible to Receive It?
Aug. 20, 2021 - Katie McCallum12/29/2021 UPDATE: The effectiveness of two out of three of the available monoclonal antibodies for COVID-19 is greatly reduced against the predominant omicron variant. After a temporary pause while waiting for supply, Houston Methodist has resumed its monoclonal antibody infusions with Strovimab, which has shown to be effective against the COVID-19 omicron variant. Due to limited supply, at this time we will only be able to refer patients who are immune compromised or over the age of 65 with a risk factor.
When the pandemic first began, no specific treatment for COVID-19 existed. Since this time, however, the FDA has granted Emergency Use Authorization (EUA) to several monoclonal antibody therapies as a treatment for COVID-19.
"For the first eight months of the pandemic, there was very little that clinicians could do for those who tested positive for COVID-19 but did not require hospitalization — beyond taking a wait-and-see approach, explains Dr. Howard J. Huang, medical director of the Houston Methodist Lung Transplant Center. "If a person's symptoms became severe, we could at that point manage and treat the resulting complications via oxygen therapy and other methods. But, the ideal scenario is to prevent severe symptoms from ever developing in the first place."
With monoclonal antibody therapy, physicians now have a way to help prevent severe symptoms from developing in those who are high risk.
More recently, the FDA extended the potential application of monoclonal antibody therapy for preventive use in those at risk due to a confirmed exposure to the virus. The authorization was based on the results of a large clinical trial that found the antibodies prevented symptoms in household contacts of people who recently tested positive. The FDA stressed that the therapy is not a substitute for vaccination, however.
Dr. Huang is here to answer the common questions you may have about monoclonal antibody therapy for COVID-19.
How does monoclonal antibody therapy work?
Dr. Huang: Monoclonal antibody (mAb) therapy, also called monoclonal antibody infusion treatment, is a way of treating COVID-19. The goal of this therapy is to help prevent hospitalizations, reduce viral loads and lessen symptom severity.
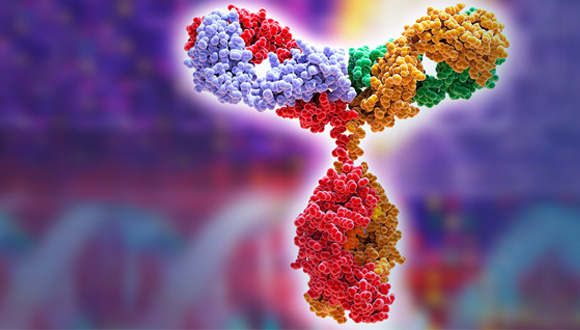
This type of therapy relies on monoclonal antibodies. These are antibodies that are similar to the ones your body would naturally make in response to infection. However, monoclonal antibodies are mass-produced in a laboratory and are designed to recognize a specific component of this virus — the spike protein on its outer shell.
By targeting the spike protein, these specific antibodies interfere with the virus' ability to attach and gain entry into human cells. They give the immune system a leg up until it can mount its own response.
This therapy can be extremely effective, but it's not a replacement for vaccination. The community still needs to step up and get vaccinated to break the virus' chain of transmission.
Who is eligible to receive monoclonal antibody therapy?
Monoclonal antibody treatment is available to individuals who:
- Are high risk** for developing severe COVID-19 AND
- Have a positive COVID-19 test and have not yet been admitted to the hospital AND
- Are 12 years of age or older (and at least 88 pounds)
Post-exposure preventive monoclonal antibodies are available to those who have been exposed (consistent with the CDC's close contact criteria)* AND who are:
- High risk** for developing severe COVID-19 AND
- Not fully vaccinated OR vaccinated but immunocompromised AND
- 12 years of age or older (and at least 88 pounds)
*In some cases, direct exposure isn't a criterion. If you meet the criteria above and are at high risk of exposure to an individual infected because of an occurrence of infection in other individuals in the same institutional setting (for example, nursing homes or prisons), you are eligible for post-exposure preventive monoclonal antibodies.
It is important to understand that post-exposure preventive monoclonal antibodies are not a replacement for vaccination. We highly encourage everyone to get a COVID-19 vaccine.
**High risk includes any of the following:
- 65 years of age or older
- Overweight (body mass index over 25)
- Pregnancy
- Chronic kidney disease
- Diabetes (Type 1 and Type 2)
- Weakened immune system
- Currently receiving immunosuppressive treatment
- Cardiovascular disease/hypertension
- Chronic lung disease
- Sickle cell disease
- Neurodevelopmental disorders
- Medical-related technological dependence
Do I still need monoclonal antibody therapy if I'm not feeling sick yet?
Dr. Huang: For monoclonal antibody therapy to be most effective, it needs to be taken as early in the disease course as possible. So, the sooner the better — even if you're not feeling that bad yet.
In high-risk patients, receiving treatment earlier, when symptoms are less severe, may help prevent progression of the disease that would otherwise require hospitalization.
How is monoclonal antibody therapy administered?
Dr. Huang: Monoclonal antibody therapy is given through intravenous (IV) infusion. These infusions are given in one of our outpatient infusion centers and require about an hour to administer, followed by an hour of observation and monitoring.
One possible side effect of monoclonal antibody therapy is an allergic reaction. These reactions typically only occur during infusion or soon after, and your care team will closely monitor for any signs of an allergic reaction. However, because an infusion reaction can also be delayed, contact your doctor immediately if you notice any of the following signs of an allergic reaction:
- Fever and/or chills
- Nausea
- Headache
- Shortness of breath
- Low blood pressure
- Wheezing
- Swelling of lips, face or throat
- Muscle aches
- Hives or itchiness
When administered for preventive use, monoclonal antibody therapy can be given as a subcutaneous injection.
Does receiving monoclonal antibody therapy mean I can cut my isolation short?
Dr. Huang: Anyone who has tested positive for COVID-19 needs to isolate — regardless of whether or not he or she has received monoclonal antibody therapy.
Only after meeting the CDC's isolation criteria can you return to work and leave your home (while still social distancing and wearing a mask).
Can I receive monoclonal antibody therapy if I'm pregnant or breastfeeding?
Dr. Huang: Because there's very limited data regarding how this therapy affects pregnant women and unborn babies, the risk of this new therapy may outweigh the benefits in some cases. If you are high risk and develop COVID-19 while pregnant or breastfeeding, it's important to discuss your treatment options and your specific situation with your doctor.
Is there anything I need to know about receiving monoclonal antibody therapy?
Dr. Huang: After receiving monoclonal antibody therapy, it's recommended that you wait 90 days before receiving the COVID-19 vaccine. If you already received the first dose of vaccine before monoclonal antibody therapy, current CDC guidelines recommend you wait 90 days before receiving the second dose.