You pick up a package on your doorstep — and you're surprised by how heavy it is, but you manage it anyway. The next thing you know, the dull ache in your lower back suddenly turns into a sharp pain running down the back of your leg.
Could it be a herniated disk?
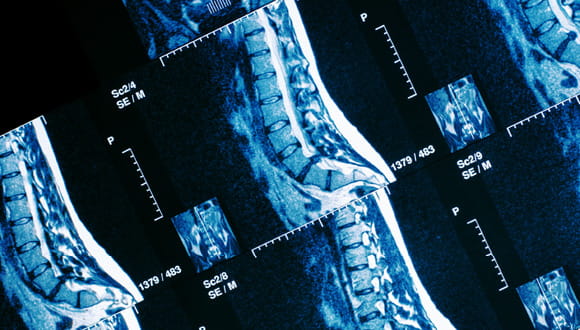
"Disk pain is often the result of a gradual, age-related wear and tear called disk degeneration," explains Dr. Karl Vega-Lelkes, orthopedic spine surgeon at Houston Methodist. "A herniated disk in the lumbar or lower back is common, but disks in the neck can also slip or herniate. The thoracic or mid-back discs are rarely affected."
What are the symptoms of a herniated disk?
The spinal column consists of vertebrae separated by softer, cushiony disks. A herniated disk occurs when that softer material slips outside the vertebral column and presses against spinal nerves causing pain. These disks act as shock absorbers, but when they are compromised, symptoms can develop.
Common symptoms of a herniated disk include:
- Arm pain, leg pain or lower back pain, depending on the location of the affected disc, that can radiate from the buttock to the foot or through the shoulder and arm
- Numbness or tingling in the limb that is served by the nerve the disk is pressing against
- Muscle weakness impacted by the affected nerve, causing you to stumble or have difficulty lifting or holding items
- Neck pain or low back pain that worsens with activities that involve bending or lifting
- Pain that intensifies when sneezing or coughing
(Related: 5 Signs It's Time to See a Spine Specialist)
What are the risk factors of having a herniated disk?
A herniated disk can occur for a variety of reasons, but certain factors can increase risk. These include:
- Age: Disk degeneration is a natural part of aging, making herniation more common in middle-aged and older adults
- Genetics: A family history of disk problems can make a person more prone to experiencing similar issues
- Improper lifting technique: Lifting heavy objects without proper posture places undue pressure on the spine, heightening the risk
- Inactivity: Long periods of sitting or lack of regular exercise can weaken muscle strength and reduce spinal stability
- Occupation: Jobs that involve repetitive lifting, pulling, bending or twisting can strain the spinal column and contribute to disk herniation
- Weight: Excess body weight adds stress to the spine, particularly the lower back, increasing the likelihood of disk issues
How is a herniated disk treated?
"Treatment varies based on your overall health, age, activity level and severity of the symptoms. Initially a short period of rest and pain medications, such as anti-inflammatory drugs or painkillers, may be followed by physical therapy," explains Dr. Vega-Lelkes.
Taking into consideration your condition and medical history, physical therapists may combine exercise with the following treatment options:
- Bracing of the neck or lower back
- Electrical stimulation
- Heat or ice treatment
- Traction (a mechanism to pull a vertebrae back into place and hold it there)
- Regular physical exams to monitor progress
As the pain improves, physical therapists will teach you core-strengthening exercises to increase muscle strength and help avoid a recurrence. Generally, most people's symptoms improve within a month of nonsurgical treatment.
"If physical therapy doesn't provide relief, steroid injections may help control the pain," Dr. Vega-Lelkes adds.
These injections, given in the doctor's office, reduce swelling around the spinal cord or herniated disk to relieve symptoms. Your doctor may use X-ray, CT scan or fluoroscopy to locate the affected area where an injection is needed.
When is surgery needed to fix a herniated disk?
"For patients whose symptoms do not subside with other treatments, surgery may be necessary," Dr. Vega-Lelkes says.
Your doctor may recommend spine surgery if:
- Symptoms haven't improved after six weeks of conservative treatment
- A disk fragment lodges in your spinal canal and presses on a nerve, causing progressive weakness
- You have difficulty performing basic daily activities, such as standing or walking
- The outer ring of the disk has ruptured
In most cases, the surgeon removes the protruding section of the disc. Rarely, the entire disk must be removed and the vertebrae must be fused with metal hardware to stabilize the spine. Your surgeon could also suggest implanting an artificial disc. In cases where nerve damage or cauda equina syndrome occurs, prompt surgical intervention is important.
What does recovery from a herniated disk consist of?
Recovery often includes avoiding lifting heavy objects, practicing regular exercise and maintaining a healthy weight to prevent future herniation. Over-the-counter pain relievers, such as ibuprofen or other anti-inflammatory medications, can help manage discomfort and reduce swelling. Your healthcare provider may also recommend short-term bed rest to ease pressure on the affected part of the spine and allow the body to begin healing.
It's important to stay attentive to your symptoms during recovery. If pain is worsening despite rest and medication, or if new symptoms develop, consult your health care provider immediately. A comprehensive recovery plan, including physical therapy, stretching exercises and proper movement techniques, can significantly reduce the risk of further injury and help restore your quality of life.