Diabetic Retinopathy Expert Presents New Results from KSI-301 Trial at AAO
Oct. 6, 2023 - Eden McCleskeyA Houston Methodist ophthalmologist and leading diabetic retinopathy researcher, Dr. Charles Wykoff, will present first-time clinical trial data from the Kodiak GLOW-3 trial at the American Academy of Ophthalmology Annual Meeting on Nov. 3, 2023.
Dr. Wykoff will announce outcomes from the randomized, controlled phase 3 trial of tarcocimab tedromer (KSI-301), a novel intravitreal anti-VEGF treatment for diabetic retinopathy engineered for extended durability.
“Medicine that is able to be given at meaningful longer intervals could help patients and physicians better realize the long-recognized potential of anti-VEGF therapy as a preventive treatment for non-proliferative diabetic retinopathy,” Dr. Wykoff said in a press release announcing enrollment in the trial was complete.
It’s been a busy and exciting year for retinal disease researchers, particularly Dr. Wykoff, who leads multiple national clinical trials assessing emerging therapies and new diagnostic technologies.
Study identifies biomarkers predictive of worsening diabetic retinopathy disease
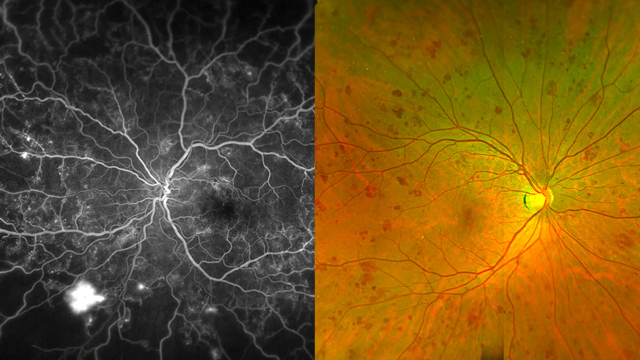
Earlier this year, a study by Dr. Wykoff and colleagues found that predominantly peripheral lesions (PPLs) and retinal nonperfusion detected by ultra-widefield fluorescein angiography (UWFA) were early warning signs that a person's diabetic retinopathy is at risk of meaningfully worsening and requires closer follow-up and care.
The study marked the culmination of a decades-long search to identify and validate novel biomarkers to help predict progression to more severe, vision-threatening forms of the disease in order to guide clinical care delivery and management.
"Our aim was to assess the clinical relevance of PPLs, including hemorrhages and other signs of diabetic retinopathy located in the retina periphery, using the two forms of relatively new technology that allow us to consistently image them: ultra-widefield color fundus photography and ultra-widefield fluorescein angiography," Dr. Wykoff said.
The study, published in JAMA Ophthalmology, found that the presence of PPLs on UWFA was associated with a 1.7-fold greater risk of disease worsening over four years (P < .001), independent of baseline severity scores. No association was identified with color fundus PPLs.
Retinal nonperfusion — impaired blood flow as detected by UWFA — was also associated with increased risk. Nearly half (46%) of those in the highest retinal nonperfusion quartile and roughly a quarter (26%) of those in the lowest nonperfusion quartile met the primary endpoint of disease worsening within four years.
"These results suggest that the use of ultra-widefield fluorescein angiography can enhance the clinician's ability to predict disease worsening while the patients are still in the non-proliferative stage," Dr. Wykoff said. "It supports a role for UWFA in future staging systems and clinical care."
As a result of the study, a national panel of leading opthalmologists is currently revising the Diabetic Retinopathy Severity Scale to incorporate guidance about UWFA.
Diabetic retinopathy is a common complication of diabetes mellitus, affecting over one third of people diagnosed with the blood sugar disorder. It leads to visual loss through diabetic macular edema, proliferative diabetic retinopathy and retinal nonperfusion.
"There has been long-standing interest in identifying biomarkers to help predict disease worsening," Dr. Wykoff said. "Many patients remain in the non-proliferative stage for an extended period of time, during which they are often relatively asymptomatic. While it may not be clinically indicated to treat all of these patients with ocular-specific interventions, there is a risk of patients transitioning to a more advanced stage of the disease and incurring irreversible damage before one realizes it's time to intervene."
Incorporating data on 544 eyes collected from 37 Diabetic Retinopathy Clinical Research Network (DRCR) sites across North America, the JAMA Ophthalmology study is a large-scale follow-up to research published in 2015 that reported the association between PPLs and progression to more severe forms of disease.
The new study largely validates the prior research, but only for UWFA-associated PPLs.
"The dye-based UWFA study is slightly more invasive but also more sensitive at identifying anomalies in blood flow and peripheral pathology that may be indicative of worsening disease," Dr. Wykoff explained.
In the past decade, the emergence of ultra-widefield imaging has allowed 90% of the retina to be directly captured with imaging, a meaningful improvement over standard retinal photographs and fluorescein angiography, the longstanding diagnostic tools. Those only capture about a third of the retina, centered on the posterior pole.
"Ultra-widefield technology is not available everywhere and is not necessary for providing excellent management, but it is emerging as an important means of prognosticating and following disease progression carefully," Dr. Wykoff said. "Providers should consider incorporating it and facilitating access, as appropriate, for patients interested in the extra insight it can provide."