Breast Cancer Recurrence Score Predicts Benefits of Radiation Therapy
April 12, 2023 - Eden McCleskeyFor over a decade, clinicians have used the 21-gene RT-PCR recurrence score, commonly referred to as Oncotype or Oncoscore, to determine which early-stage breast cancer patients should receive chemotherapy after breast-conserving surgery and which patients can safely omit it.
Now Houston Methodist researchers have extended the test's applicability even further — using it for the first time to determine if early-stage breast cancer patients can safely skip radiation therapy as well.
A Houston Methodist study, published recently in Practical Radiation Oncology (PRO), found that radiotherapy improved survival rates among patients with intermediate to high recurrence scores but did not impact survival rates in patients with low recurrence scores.
"This test has helped us personalize the treatment journey and improve quality of life by reducing the number of patients exposed to toxic therapies which have minimal clinical benefit for them," says Dr. Bin Teh, vice chair of Radiation Oncology at Houston Methodist and principal investigator of the PRO study. "It only makes sense to find out if it can help us personalize radiation therapy as well."
A large national prospective clinical trial is currently under way, but its findings are not expected to be released for several years.
To provide insight and clinical guidance in the interim, Dr. Teh and a team of researchers analyzed the recurrence scores and medical records of nearly 80,000 patients with hormone receptor positive, HER2 negative, nonmetastatic invasive breast cancer. The results were published in the PRO study.
"Patients with this diagnostic profile — about 70% of new cases in the U.S. — are typically early stage and lower risk, which is why we're looking at their oncoscores to see if there are any treatments we can safely omit," says Dr. Teh. "The other 30% of patients have more aggressive variants or cancer that's at a more advanced stage and less leeway with how to proceed. There's no decision to help them make."
In the study, 24% of participants were categorized as low risk (RS = 1-10), 66% as intermediate risk (RS = 11-25) and 10% as high risk (RS = 26-100). Radiotherapy was found to produce statistically significant improvements in survival rates for those at intermediate (P = .001) and high risk (P < .001). No survival benefit was observed for those at low risk (P = .184).
"Although it's nice to know that some very low-risk patients may have additional flexibility based on these results, it's equally nice to confirm that the vast majority of patients significantly benefit from current radiation therapy recommendations," comments Dr. Teh.
Potential changes to radiotherapy treatment guidelines will impact significantly fewer patients than similar studies on chemotherapy and recurrence scores. Those studies established that only patients in the highest risk category (post-menopausal women with RS >25 and pre-menopausal women with RS >16) should receive chemotherapy, relieving approximately 70% of breast cancer chemotherapy volume as a result.
"Although we're using the same recurrence score to make decisions for the same population of patients, the risk/reward calculus is different for these two treatments," Dr. Teh explains. "Radiation therapy is more targeted and has fewer undesirable side effects. It is also very effective in eliminating cancer cells."
In fact, Dr. Teh is careful to note that clinicians and patients should be cautious about using these findings to opt out of radiation therapy.
"Our study only took survival into account, not local regional recurrence," Dr. Teh says. "Other studies have shown that radiotherapy reduces the risk of local regional recurrence. Worrying about your cancer coming back — or having to go through surgery and treatment again — those things negatively impact quality of life as well."
According to Dr. Teh, even patients in the lowest risk category may find that the benefits of radiotherapy outweigh the drawbacks.
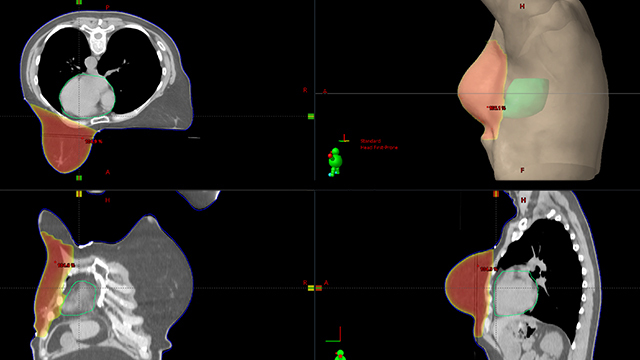
"People still have a lot of misperceptions about radiation therapy based on outdated facts, for instance that it might hurt your skin or negatively impact your heart," Dr. Teh says. "We have more advanced techniques and technologies now that allow us to achieve the best results while minimizing side effects."
It is also incredibly efficient. Typical treatment duration is three to four weeks, five days a week, for approximately 15-20 minutes. Hormone therapy — also a standard part of the breast-conserving therapy regimen — lasts for five years.
"I recently treated a breast cancer patient who was 103 years old," Dr. Teh says. "She did absolutely great. So now I tell all my patients, if she can do it, so can you."