Socially Vulnerable Counties Face Higher Premature Cardiovascular Mortality Rates
Oct. 27, 2022 - Eden McCleskeyPeople under the age of 65 who live in the nation's most socially vulnerable counties were nearly twice as likely to experience premature cardiovascular disease (CVD) mortality as their age-matched peers who live in the least socially vulnerable counties, according to a Houston Methodist study.
In socially vulnerable counties — that is, counties with significantly limited resources — Black residents had the highest risk of CVD mortality among racial/ethnic groups, and rural residents had markedly higher CVD mortality rates compared to their urban counterparts.
"Our study highlights the socioeconomic, geographic and racial disparities still prevalent in our society and their impact on overall and cause-specific premature CVD mortality," says Zulqarnain Javed, Ph.D., M.B.B.S., M.P.H, a cardiovascular epidemiologist and outcomes researcher at Houston Methodist Academic Institute and study co-author.
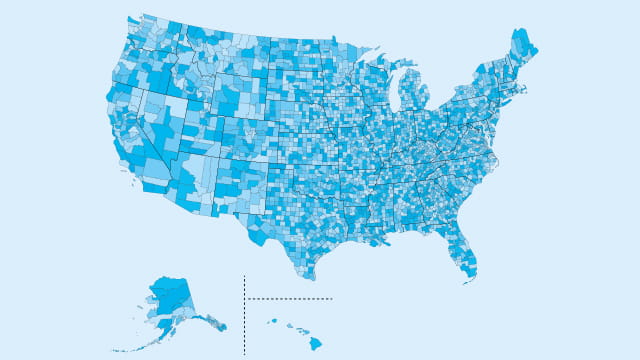
The Houston Methodist research team used the CDC's social vulnerability index (SVI) to divide all 3,143 U.S. counties into quartiles representing increasing levels of vulnerability, and analyzed premature death rates (<65 years) for ischemic heart disease, stroke, hypertension and heart failure at each quartile.
SVI ranks population groups across four themes: socioeconomic status (income, employment, education), household composition/disability status, minority status (English language proficiency) and housing/transportation.
The study, published in Circulation, further stratified results by age (18-45; 45-65), sex, race/ethnicity and county type.
The researchers found that mortality rates increased in a stepwise manner from lowest to highest SVI quartile (33.6; 43.6; 49.3; 61.8). Overall, age-adjusted CVD mortality rates were higher among middle-aged (45-65), male, Black and rural groups.
Young adults (18-45), women and people in rural counties faced double the mortality risk in the fourth versus first SVI quartile (14.5 vs. 6.9, 39.4 vs. 18.8 and 84.2 vs. 39.4, respectively). White and Black adults in the fourth SVI quartile had significantly higher rates of CVD mortality than in the first SVI quartile (56.2 vs. 32.6 and 98 vs. 62.6), with relatively smaller differences observed for Hispanic adults (31.1 vs. 23.0).
In fully adjusted models, the authors found that counties in the fourth SVI quartile had a two-fold higher risk of mortality for stroke, nearly three-fold higher risk of mortality for hypertension and over three-fold higher risk of mortality for heart failure, compared to those in the first SVI quartile. These associations were strongest for non-Hispanic Black adults and those living in rural counties.
"These findings demonstrate the importance of integrating social determinants of health into existing clinical delivery support systems and developing social risk assessment tools that may allow health care providers to better understand the structural barriers faced by socially vulnerable populations and provide informed care for improved population cardiovascular health," concludes Dr. Javed.
This post is the third in a three-part series.
Read Part 1: Social Determinants of Health and Cardiovascular Disease: What's Driving the Shift in Research?
Read Part 2: Can a Polysocial Risk Score Help Identify Individuals at Increased Risk of Atherosclerotic Cardiovascular Disease?