Small Intestinal Bacterial Overgrowth as Cause of IBS, Functional GI Disorders Lacks Evidence
July 19, 2022 - Eden McCleskeyOver the past 20 years, the advent of noninvasive, inexpensive hydrogen breath tests has made it easy and convenient to test for small intestinal bacterial overgrowth (SIBO). Maybe too easy and convenient, some clinicians worry.
SIBO diagnoses have skyrocketed since testing became widely available, and the condition is increasingly being implicated as the underlying cause of irritable bowel syndrome and a variety of other gastrointestinal and non-gastrointestinal disorders.
But whether there's scientific evidence to back up these claims is up for debate, according to a recent Gastroenterology review by Dr. Eamonn Quigley, director of the Underwood Center for Digestive Disorders at Houston Methodist, and Dr. Daniel Bushyhead, a Houston Methodist gastroenterologist.
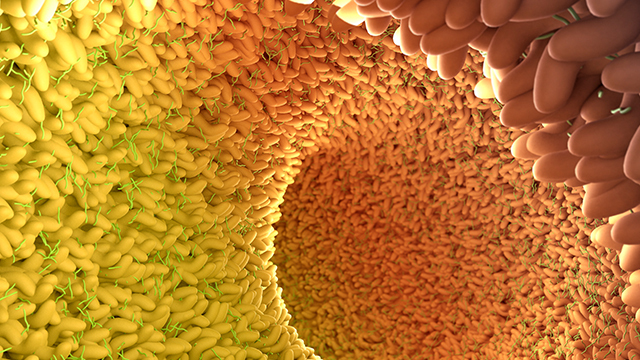
SIBO, loosely defined as "the presence of excessive numbers of bacteria in the small bowel, causing gastrointestinal symptoms," has been around as a concept for more than 80 years. But its applicability was historically limited to patients experiencing symptoms of maldigestion and malabsorption, with obvious risk factors including obstructions, surgical alterations and immune system issues that would make them more vulnerable to being colonized by potentially injurious colonic microbiota.
"The pathophysiological plausibility that underpins bacterial overgrowth as a cause of maldigestion and malabsorption is lacking in regard to its purported role in IBS," Dr. Quigley says. "We still don't know what the normal bacterial population of the small intestine should be, if bacterial overgrowth is a cause of symptoms, or how accurate these breath tests are for all patients. At this point, we still don't know which clinical disorders or diseases are truly linked to SIBO."
Dr. Quigley sat down with Leading Medicine to discuss his most recent article and key takeaways for clinicians trying to figure out how to provide care in a rapidly changing landscape.
Q: What are the main concerns you are trying to address in this piece?
First, there's this school of thought and narrative that bacterial overgrowth is responsible for a wide variety of gastrointestinal symptoms and syndromes like IBS. And what we point out in the article is that there's very little evidence to support this. Yes, there may well be a group of patients who have symptoms which overlap between IBS and SIBO, but for the vast majority of patients with IBS, there's no reason to believe SIBO is the cause of their problems. What evidence we do have points to SIBO playing a role in specific situations where normal digestive processes have broken down for whatever reason, creating an environment where contamination of the small intestine is possible. But there's no physiological explanation like that in IBS or similar idiopathic functional GI disorders. We need to conduct more randomized controlled trials and follow the evidence.
Secondly, we point out that currently there's no gold standard definition or diagnostic test for small intestinal bacterial overgrowth. There are issues with both the traditional small intestinal sampling that we used to use to diagnose it and the hydrogen breath tests currently in widespread use. The old test was invasive, with potential for contamination from the mouth and esophagus. The breath tests rely too heavily on timing of when the ingested substance is supposed to hit your colon. They don't take differences in people's motility into account. Some people, for various reasons, move material more slowly or quickly than others. For this and other reasons, these tests have significant problems with false positives and false negatives.
The third point is that we need to be careful about over-prescribing antibiotics. We need to be responsible antibiotic stewards. What we don't want is to create a situation where we're using a poorly validated clinical test, wrongly diagnosing people as having SIBO, putting them on antibiotics, seeing that they don't get better, trying another round of antibiotics and causing bacterial resistance that might create even greater problems in the future.
Finally, putting it all together, just be careful about how you use breath tests and interpret their results. In general, you should try to limit their use to conditions where bacterial overgrowth is plausible, the mechanism by which it may cause symptoms is clearly demonstrated, and treatment has been shown to be effective.
Q: What kind of conditions make small intestinal bacterial overgrowth more plausible?
The way I look at this is fairly simple. Think about what normally prevents all of us from having bacterial overgrowth. Stomach acid kills a lot of bacteria. So, any condition where your stomach acid is reduced may predispose you to SIBO. If your motility in your bowel is normal, then bacteria are moved along and don't get a chance to proliferate. But, if you have anything that leads to stagnation in the bowel — like an obstruction, fistula, motility disorder or stricture — that could promote bacterial proliferation. There are a few other things, like certain surgeries that reroute intestinal contents, or immune deficiencies that may make it harder to mount a response to normal bacteria. But if you just think about it logically, you can see which scenarios are likely to lead to bacterial overgrowth and which scenarios make bacterial overgrowth highly unlikely.
Q: Is there anything on the horizon to help us determine what is the normal amount of bacteria in the small intestine?
In recent years, we have been learning more and more about the gut microbiome with high throughput sequencing and metagenomic analyses and these technologies are just now being applied to the small intestine. We do not have enough data yet. And it may be awhile before we do because it's hard to get a sample from the small intestine. It's certainly not as easy as getting a fecal sample, which patients can provide themselves.
But there are some interesting technologies in the pipeline, or in limited use in clinical trials. There are a lot of exciting things happening with capsule technologies, similar to capsule endoscopy, which we have been using for decades and which provides excellent pictures of the digestive tract. One of these new technologies can sample the gases it encounters as it moves through the small intestines and give you a live read-out of hydrogen and other gases as it moves along. That solves the problem of the breath tests being dependent on timing without being sensitive to patients' various speeds of gut transit. We will know precisely where it is and what it's reading. I think we may even be able to use capsules to test samples while they're in the small intestine, not just read gas levels.
This is the sort of technology that could blow the whole field open. And that's why we encourage clinicians to wait a little while longer, so we all have more knowledge about what's normal and abnormal. Then we can go about assigning blame to SIBO and, better yet, solving problems.