New Insights on Subarachnoid Hemorrhage Point to Underlying Causes of Long-Term Neurological Effects
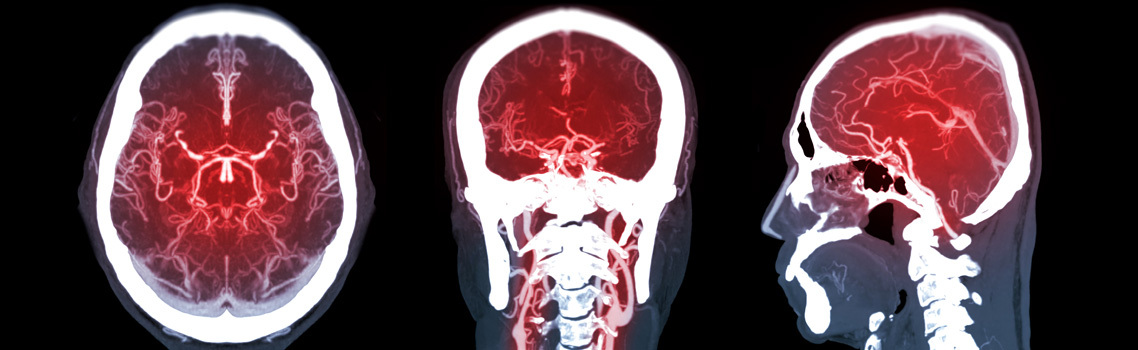
Sep. 23, 2021 - Eden McCleskeyAneurysmal subarachnoid hemorrhage is a devastating type of stroke caused by the spontaneous rupture of an intracranial aneurysm and characterized by the accumulation of blood in the subarachnoid space surrounding the brain.
Although subarachnoid hemorrhage (SAH) is relatively rare, occurring in 30,000 Americans each year and accounting for about 3% of all strokes, its complications are among the most catastrophic. Roughly a third of patients die, a third survive with significant disability and even the third who eventually recover well enough to return to their homes and jobs are usually not the same. Half of all cases occur in individuals under 55 who would otherwise have a long and productive life ahead of them.
Even those considered to have positive outcomes face permanent motor or cognitive impairment, as well as psychosocial disorders, for reasons that are not well understood and not necessarily expected based on pathophysiological studies of the post-SAH brain.
Dr. Gavin Britz, chair of the Houston Methodist Hospital Department of Neurosurgery, has long been at the forefront of researchers trying to understand the pervasive and puzzling long-term neurological side effects of SAH. He spoke to Leading Medicine about his team's most recent discoveries and his presentation at the American Academy of Neurological Surgery Annual Scientific Meeting on Sept. 24.
Q: Could you provide some background about your interest in subarachnoid hemorrhage?
About 95% of people who survive aneurysmal SAH say they are never the same again. They report that their memory, judgment and executive function are not as good as before — and those are some of the most critical things that we need to get along in this world and that make us who we are. This is true even in those with the best outcomes, the ones who recovered relatively quickly and didn't suffer paralysis, weakness or any of those major physical impacts of stroke.
So even those patients have significant deficits and, the interesting thing is, no one really understands why. We understand that people can have deficits as a result of injury to the brain tissue, hydrocephalus, the hemorrhage itself, but even when you take away those patients, the patients that are expected to have a normal result are still not the same.
Q: So it's a mystery you're hoping to solve. What are some of the theories you've investigated?
Initially, my work in the lab was focused on the large circulation blood vessels that might be causing these neurological deficits. But that only occurred in one in five patients.
When I was in Seattle, we began to focus on microcirculation — looking at the small vessels and trying to find out if they are abnormal and characterizing how and why they are abnormal. We found that, yes, microcirculation is abnormal, but it still doesn't explain everything.
When I was at Duke, we focused on the hippocampus, which is where the executive function is, and partnered with some of the epilepsy surgeons. We found that, yes, clearly the area was abnormal as well, in regard to function and how it responds to circulation. So obviously the microcirculation is connected, but still no one's really figured out how and why this happens.
There are several researchers looking at inflammation microthrombi in the blood vessels. And I really believe that plays a role, but I also think that it's more than that.
The hippocampus is within the brain, and it's well protected. So why would blood that's outside the brain affect the hippocampus inside? And that's been the whole focus of my lab since coming to Houston Methodist in 2013.
Q: What are your most recent studies showing?
We are now very clearly showing that the blood on the outside of the brain stimulates the perforant pathway, which leads from the entorhinal cortex into the hippocampus. That pathway is then damaged by an immune response called the complement. We all need the complement to keep us alive. But when any immune response overreacts, or gets out of control, it results in damaging the thing it's trying to protect.
In this case, it results in a pruning of the dendritic spines which leads to myelin loss. And, of course, myelin loss is associated with dementia, Alzheimer's and the sort of cognitive deficits that we see in patients with subarachnoid hemorrhage.
Q: So you think there's a chain reaction triggered by blood being where it's not supposed to be?
Essentially, yes. It's not the aneurysm causing a direct hit in the brain, leading to cell death and loss of function. It's a multifactorial process that occurs over time. One of the interesting things about these SAH cases is that there's no cellular loss in the hippocampus, which we might have expected to see. The hippocampus does get smaller over time. There is atrophy. But it's not because of cellular loss.
What we're showing now is that it's due to myelin loss and dendritic pruning. In a paper published this summer, we looked at how the hippocampal transcriptome changes after SAH. The genes that were clearly expressed were the ones involved in inflammation, complement and myelin, so it makes sense and confirms what we've been seeing.
The picture is beginning to get much clearer, and we're getting closer to understanding why people with SAH have these lifelong cognitive effects. And that's important because it could lead to interventions, treatments and hopefully a return to normalcy for these patients who have already been through this surprising, traumatic, life-threatening event.