CAC Score and Atherosclerotic Cardiovascular Disease Risk Assessment: Can a Test Predict the Future?
Sep. 10, 2021 - Eden McCleskeyUnless your clinic or exam room features a working crystal ball, it's difficult to predict accurately which patients will suffer an atherosclerotic cardiovascular disease (ASCVD) event.
That's because traditional risk factors like age, weight, blood pressure and cholesterol levels can help estimate a person's risk, but they don't measure the actual burden of disease: the coronary atherosclerotic plaque, the main underlying cause of coronary events.
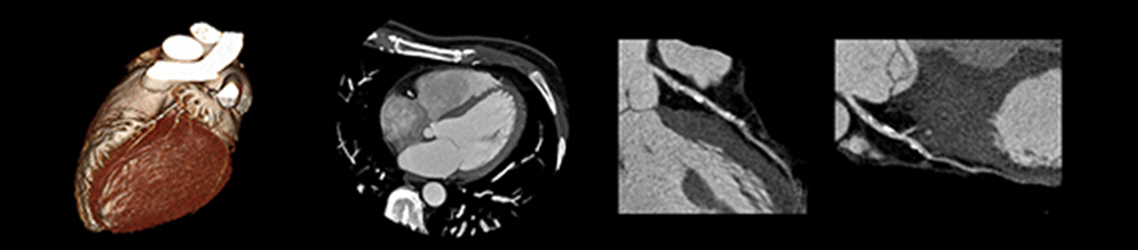
For that, you need a coronary artery calcium, or CAC score, which you get by looking inside the arteries using a relatively inexpensive, low-radiation, non-contrast computed tomography (CT) scan.
In a recent review published in the British Medical Journal, Houston Methodist cardiologists Drs. Khurram Nasir and Miguel Cainzos-Achirica discuss the history of the CAC test, key studies leading to its adoption in clinical practice guidelines and its role in the personalization of risk scoring and subsequent management strategies.
"CAC is very useful in that it allows us to stop guessing about our patient's risk and get an actual measurement of their burden of coronary plaque," Dr. Cainzos-Achirica says.
Today, more than 30 years after the inception of the score, there is ample support to continue using CAC as a decision aid in the prescription of statins and potentially other preventive medications and interventions as well.
"There is now overwhelming evidence that CAC presence is the strongest predictor of short- and long-term risk for ASCVD," Dr. Nasim says. "Many individuals considered to be very low risk actually have elevated CAC and, as a result, are at higher risk for heart disease and stroke. And vice versa — an estimated one-third to half of those who are in traditionally higher risk categories actually have no CAC and are subsequently much lower risk than anticipated."
Knowing the difference is critically important for downstream decision-making and for identifying those patients who need more aggressive management versus those who have more flexible treatment choices. That could mean refraining from, or at least delaying, expensive novel therapies, especially if the patient's calcium score is zero.
The power of zero
In an early publication on the subject, Dr. Nasir coined the term the power of zero about calcium scores, a reference to the fact that patients with a CAC count of zero have very low rates of cardiovascular events during follow-up — or at least the lowest among their cohort.
For instance, a 75-year-old patient with a score of zero does not have zero risk of cardiac events but has the lowest risk among all other 75-year-olds and markedly lower risk than a 75-year-old with a high score. The same applies to patients with diabetes, severe hypercholesterolemia and other features that increase the average risk of cardiovascular events.
"What we've shown consistently with research over the past 15 to 20 years is that a CAC score of zero is a particularly powerful prognostic tool," Dr. Nasir says. "When you follow individuals over a set period, you can see that the true risk can be reflected more accurately by the presence and burden of plaque. If you don't have any plaque build-up, it means there's something about your body that's offering enhanced protection, or resiliency, from heart disease."
How long that protection lasts is a subject of ongoing debate and research, though Drs. Nasir and Cainzos-Achirica recommend that patients with a CAC score of zero get their levels rechecked every three to five years.
Additionally, it's important to understand that having a CAC score near zero and having a CAC score of zero are not the same thing.
"When you move from zero to one, that means the substrate of the disease has started," says Dr. Nasir. "Even the tiniest amount of detectable plaque raises your risk of event 2.5-fold over a person with no plaque. Which points back to why we call it the power of zero."
The benefits of de-risking
CAC zero isn't just meaningful for the patient; it's empowering for the patient's physician as well. It allows for enhanced flexibility in terms of deciding what treatments and interventions are most appropriate to keep the patient on a healthy track.
For example, if a patient in a traditionally high-risk category has a zero CAC score, you can have a nuanced discussion about taking a daily statin pill — based on lifestyle, interest, familial history, etc. — rather than just prescribing it.
"Statins are safe, relatively inexpensive and their benefits are large in people at high absolute risk," Dr. Cainzos-Achirica says. "But in people at low risk, evidence shows the benefits are very small, if any. Taking a medication daily for 10 years when it is not going to yield significant benefit may not be desirable for many patients, and in a context of precision medicine, CAC can help inform those discussions."
A similar reasoning applies to other interventions, with the added consideration of potentially large out-of-pocket costs.
Novel medications such as GLP1 receptor agonists for patients with diabetes or PSK9 inhibitors for patients with severe hypercholesterolemia can cost thousands per year, even with insurance. If the patient has very high CAC, the absolute reduction of risk can be dramatic with these interventions. But, if the patient has zero CAC, the reduction in absolute risk will be more modest.
"Our studies in the field of financial hardship in cardiovascular patients in the U.S., led by Dr. Nasir, show that many patients in the U.S. are reporting so-called financial toxicity caused by the cost of care from cardiovascular disease and certain associated risk factors like diabetes," Dr. Cainzos-Achirica says. "Also, health care expenditure continues to increase in the U.S. and elsewhere. In this context, it's important to route the right resources to the people who really need them, and to try to be as precise in our management as we can."
The future of preventive care: Is CAC the new crystal ball for ASCVD risk?
Over the last several decades, mortality rates for cardiovascular disease have improved, thanks to improved prevention and enhanced treatments. However, it remains the No. 1 cause of death for both men and women across ethnic groups.
An accurate assessment of risk is crucial to the prevention of the disease.
"Low risk means flexibility — you can avoid the medicine right now and focus on lifestyle, or you can take just a small dose of the medication," says Dr. Nasir. "Conversely, if your CAC score reveals you have a high burden of plaque, you know you have to be very aggressive. Here's exactly how aggressive you need to be. It's like GPS for your risk."
Studies conducted by Dr. Nasir, among others, suggest that patients are more compliant when they have an accurate picture of their burden of plaque. It improves adherence to both lifestyle changes and medication to know how much is riding on these interventions.
"We are seeing a shift from risk factors to a paradigm in which we see disease and treat disease," says Dr. Nasir. "In preventive cardiology, the calcium score is a really important part of this. It's being adopted — a little more slowly than we'd expect — but at Houston Methodist we believe in leading medicine. Using CAC to inform the best and most personalized management of our patients is one way we can do that. Our focus will continue to be on bringing new research into this space and getting the word out to both patients and physicians alike."