Muscle-Invasive Bladder Cancer Trial Breaks New Ground with In Situ Vaccine Therapy
Nov. 22, 2022 - Eden McCleskeyImmunotherapy isn't an obscure newcomer anymore. With more than 1,000 active clinical trials in the U.S. and an estimated global market of over $200 billion, it has officially arrived.
That only 20 percent of cancer patients respond to current immunotherapies, however, means the revolution that was promised still has a long way to go.
A new clinical trial for muscle-invasive bladder cancer, currently underway at Houston Methodist, is hoping to radically speed things up by taking a novel approach to one of the oldest immune therapies on the books — vaccines.
The trial is one of the first to study the efficacy of combining an immune checkpoint inhibitor with radiation therapy to create an in situ vaccine for bladder cancer — a leading cause of cancer deaths among men and women.
Immunotherapy evolved
In situ vaccination is a cutting-edge strategy in cancer research that aims to activate an immunological response inside the tumor itself through local administration of an immunomodulatory agent.
The therapeutic vaccine is generated in vivo, bypassing the need to identify and isolate the specific tumor-associated antigens prior to the administration of the therapy.
"The idea is to give patients a specific, well-tolerated dose of stereotactic body radiation therapy to induce cell death within the tumor, leading to the release of tumor-specific antigens and the activation of tumor-specific T-cells, helping the immune system recognize and attack both local and distant cancer cells," explains Dr. Raj Satkunasivam, a urologic oncologist at Houston Methodist and principal investigator for the trial.
The approach is significantly less resource-intensive than attempting to create a custom cancer vaccine in a lab, a process hindered by the wide variability of tumor-associated antigens within different patients, different tumors and even within individual tumors themselves.
In situ vaccination has been explored in a handful of early clinical trials across several tumor types, but the Houston Methodist trial is the first to investigate its use in muscle-invasive bladder cancer.
A much-needed option
Patients diagnosed with muscle-invasive bladder cancer typically have a poor prognosis, especially those who are ineligible to receive neoadjuvant cisplatin-based chemotherapy due to advanced age or frail condition. For this population, the current standard of care is radical cystectomy alone followed by systemic chemotherapy at the time of disease relapse.
"Waiting for a relapse to happen and knowing there's a high likelihood of it spreading to other locations — there is a pressing need to find more effective therapies for these patients," Dr. Satkunasivam says. "On top of that, a radical cystectomy has significant morbidity and life-changing impact."
Although the current trial is not designed to replace the need for a radical cystectomy, the hope is that the treatment will produce a pathological complete response in many patients, leading to future studies and recommendations aimed at preserving the bladder while still achieving distant cancer control.
Releasing the immune system's brakes
In addition to using radiation to create an in situ vaccine, the researchers are also administering an immune checkpoint inhibitor to help overcome the immunosuppressive nature of the tumor microenvironment.
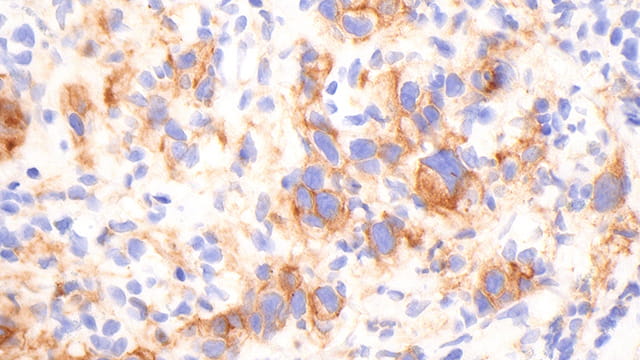
Bladder cancer is known to use the PD1-PDL1 pathway to inhibit immune cells from attacking the tumor.
Sasanlimab is an anti-PD1-PDL1 agent that potentially reactivates T cells that have been "turned off."
"This trial uses a two-pronged approach to maximize the odds of achieving effective cancer control," Dr. Satkunasivam says. "Radiation trains the body to recognize the cancer cells as a threat and sasanlimab restores the immune system response to its full power. Our goal is to create a surveillance system that seeks and destroys any bladder cancer cells, even microscopic ones that we can't see, reducing the chance that these patients will relapse in the future."
Of any form of cancer, bladder cancer has the highest chance of returning — between 50-80 percent. Risk factors include smoking and exposure to carcinogens, with higher rates found among firefighters, house painters and workers in chemical, rubber and textile plants. It is most commonly diagnosed between the ages of 75-84.
Although the study is underway, Dr. Satkunasivam estimates that enrollment will remain open through late 2023. The researchers are recruiting cisplatin-ineligible patients as well as patients who have refused chemotherapy for quality-of-life reasons.
"There are a lot of great reasons to participate in this study, or to refer a patient for it," Dr. Satkunasivam says. "We're the only ones offering it; there's likely a much better side effect and safety profile for these therapies vs. chemotherapy; and sasanlimab is administered subcutaneously and can be given quickly, unlike an infusion."