Peripheral Artery Disease: Can Advanced Imaging Tools Personalize Treatment?
March 4, 2022 - Todd AckermanHouston Methodist scientists are working with advanced imaging tools in an effort to better personalize treatment for peripheral artery disease (PAD), the sometimes fatal circulatory problem in which narrowed arteries reduce blood flow to the limbs.
The research involves the use of such technology as the 7-Tesla MRI to characterize PAD lesions and identify patients who are good candidates for minimally invasive procedures, as well as patients who should go directly to bypass surgery, a determination that's currently a huge challenge for doctors.
"Right now, there's a high failure rate in the treatment of the disease because there's no good way to predict the most appropriate interventions," says Dr. Trisha Roy, a Houston Methodist vascular surgeon-scientist and leader of the research effort. "We're very hopeful our research can change the standard of care and make a global impact on an understudied but important disease process."
Dr. Roy adds that the research has the advantage of immediate translation to the operating room because the devices being tested are already approved for use. She notes that if the research determines something works in a subset of patients, it can be adopted without regulatory steps.
Dr. Roy's team already has had conversations with the head of the European Vascular Society about incorporating its discoveries into future PAD guidelines. Such incorporation will require the collection of more data validating the team's research.
Peripheral artery disease is usually a sign of plaque buildup in the arteries. While some people with the condition have mild or no symptoms, many have leg pain when walking, most commonly in the calf. In worst cases, the condition can result in leg amputation or death.
Lower-extremity PAD affects about 10 million Americans, mostly diabetic end-stage renal disease patients, but also people with atherosclerosis stemming from hypertension, high cholesterol or smoking. In the most severe cases, known as critical limb ischemia, amputation is necessary within one year in 20% of patients. Such severe cases are the research focus of Dr. Roy's team.
Research needed because of PAD knowledge gaps
Concerned about the recent increase in such leg amputations — there are now about 150,000 a year in the U.S. — the American Heart Association last year called for a 20% reduction in the rate by 2030. The appeal, made to policymakers in regulatory bodies and health institutions, emphasized the need for greater preventive, diagnostic and research efforts. The association estimates that 85% of the amputations are actually preventable.
More research is needed because of the huge gaps in knowledge about PAD's indications or even what's happening in the blood vessels. The latter is because vessel walls aren't visualized in current imaging, only their insides, or lumens.
Blood vessels are treated by inflating balloons inside blood vessels to open them. After treating vessels, the lumens can look wide open, but give doctors a false impression because they cannot see the damage that balloon injuries can cause to the blood vessel wall during procedures.
In addition, PAD lesions are usually different than those typically seen in coronary disease. Often referred to as "Monckeberg Sclerosis," PAD lesions have a distinct pathophysiology, morphology and composition not fully appreciated, and the devices being used to treat them were never intended for the purpose.
"All the devices and techniques available to use in the leg are actually coronary devices," says Dr. Roy. "They were optimized to manage disease in the heart, and we are just applying them to the leg. The problem is that the two conditions are entirely different disease processes."
The bottom line: Doctors have to re-intervene on 75% of patients treated for disease below the knee, the most common and fastest growing PAD population requiring intervention. Dr. Roy notes those outcomes — 20% of such patients still lose their leg in a year — show the inadequacy and lack of durability of current PAD procedures.
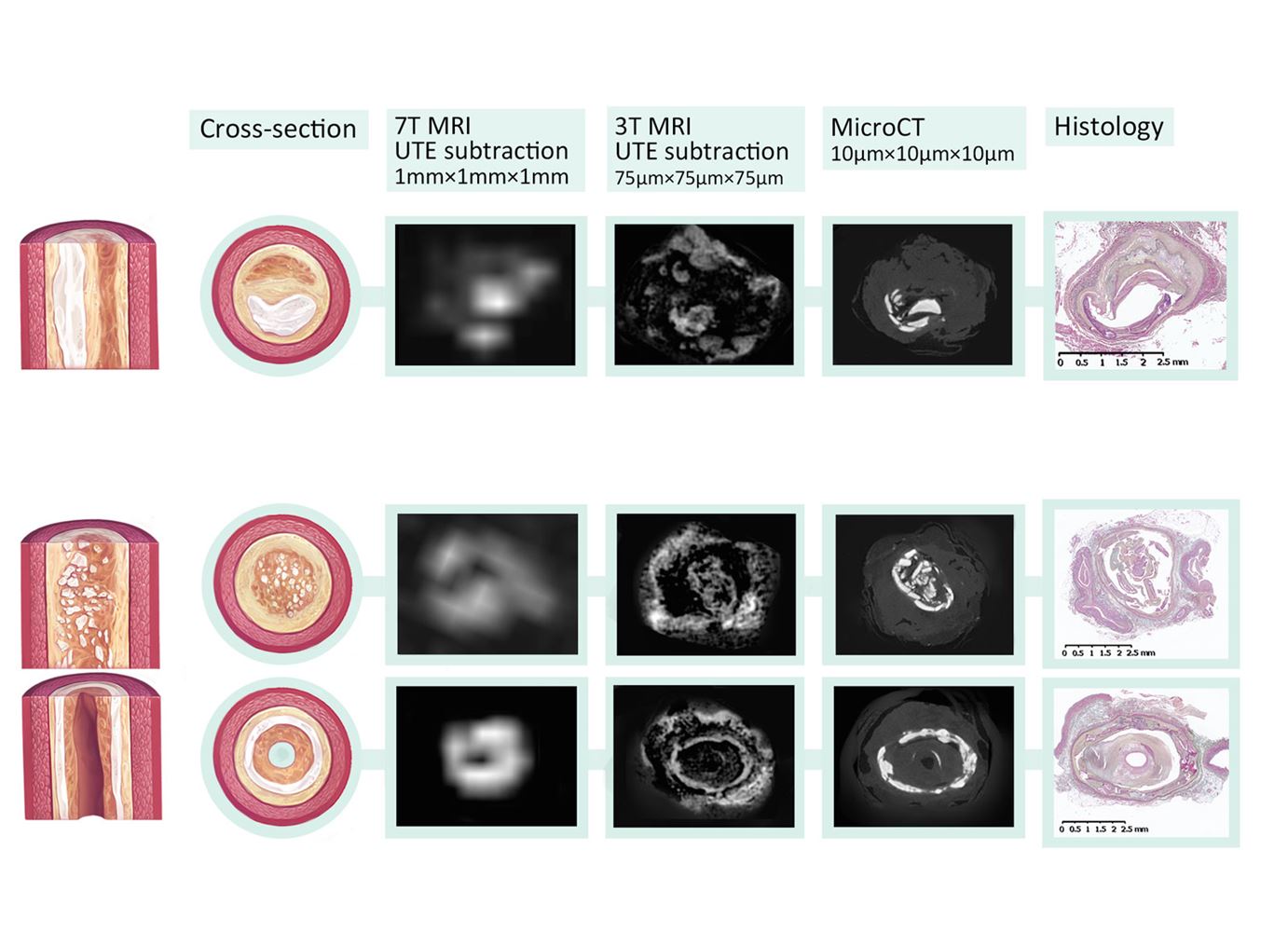
Future of better PAD diagnosis: 7-Tesla MRIs
That's where the 7-Tesla MRI comes in, thanks to its superior ability to tease apart blockages in blood vessels about 2 mm in diameter. PAD doctors currently use ultrasound and CT angiograms, which have limited ability to characterize lesions below the knee for definitive treatment planning and device selection. When MRIs are used, they are typically 3-Tesla scanners, which obtain a resolution of about 1 mm isotropic, insufficient to conduct histologic level characterization of the plaques. The 7-Tesla MRIs' much higher resolution imaging modality provides a very detailed analysis of the plaques' morphology.
The technology is not widely accessible — about 30 U.S. healthcare centers have 7-Tesla MRIs, Houston Methodist the only one in Texas. But Dr. Roy believes they are the future of PAD diagnosis, even if no one else besides her is exploring the application. She notes that the technology, primarily used in neurology thus far, is well-suited for leg imaging because vessels there, unlike in the heart, don't move.
So far, Dr. Roy's team has conducted five studies and scanned 40 patients using various PAD-imaging technologies and techniques — enough to submit an R01 grant to the NIH.
One of the studies involved testing alternative devices on amputated legs — research that showed angioplasty is often not effective, that it sometimes even destroys the peripheral blood vessel, and that preparing the vessel beforehand protected the vessel wall. A parallel study, imaging patients prior to their interventions, identified the lesions for which the standard treatment of angioplasty wouldn't have worked.
Dr. Roy notes that surgeons currently use angioplasty for peripheral artery disease — to open peripheral blood flow, to heal wounds, to ease pain or to decrease the need for amputation — but there are actually other options available to them such as atherectomy (artery removal) or lithotripsy (a non-invasive procedure involving the physical destruction of hardened masses like kidney stones).
"Those are just a couple of the options," says Dr. Roy. "The problem is, we don't know which patients will make good candidates to use these different procedures instead of angioplasty. But for now, we're treating everybody with this one-size-fits-all approach and the dismal results we're getting shows the need to personalize treatment options."