Adding Heart Failure Drug to Chemotherapy Helps Fight Triple Negative Breast Cancer
Feb. 27, 2023 - Todd AckermanThe combination of a repurposed heart failure drug and chemotherapy may benefit women with triple negative breast cancer, according to a team of Houston Methodist researchers, providing a potential breakthrough against the hard-to-treat disease.
The researchers found that the combination — the experimental drug L-NMMA and the approved drug docetaxel — reduced the size of tumors or slowed their spread in an early-stage study of patients with the often fatal condition, whose therapeutic options lag far behind more common types of breast cancer.
"This study suggests the combination could provide safer, more effective treatment than the current offerings for triple negative breast cancer," says Dr. Jenny Chang, a Houston Methodist breast medical oncologist and the study's primary investigator. "That's badly needed for a disease that, when metastatic, is still largely incurable."
Dr. Chang, director of the Houston Methodist Dr. Mary and Ron Neal Cancer Center, added that the L-NMMA and docetaxel combination represents "an effective way of cutting short drug development and getting the treatment into patients as quickly as possible." She noted the process has taken less than five years and saved billions of dollars.
The combination treatment was made possible thanks to research in Dr. Chang's lab that investigated more than 500 possible genetic markers for triple negative breast cancer (TNBC) before finding variants in a gene (RPL39) that drive the formation of the disease's most aggressive type. The lab also found that the gene works on the inducible nitro oxide signal (iNOS) pathway and can be blocked with L-NMMA, or nitro monomethyl L-arginine acetate.
Houston Methodist is licensing out the combination therapy, for which Dr. Chang is the sole inventor on a patent application (cancer treatment methods "using iNOS-inhibitory compositions"). The study, the first to investigate an iNOS inhibitor against breast cancer, was published Dec. 15, 2021, in Science Translational Medicine.
Targeting the nitric oxide signaling pathway
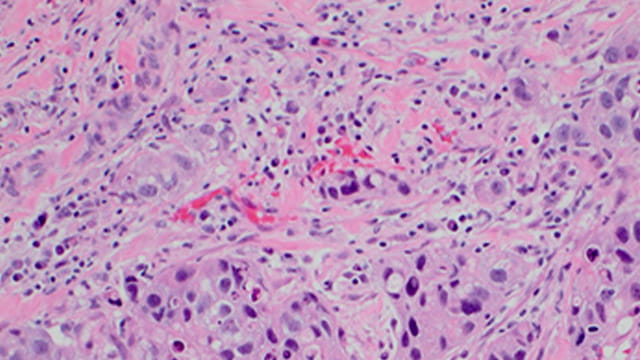
TNBC, which accounts for about 15% of breast cancers, is an aggressive form of cancer known for metastasizing quickly and becoming resistant to chemotherapy. Its five-year survival rate is 76%, compared to 90% for all breast cancers.
The disease was named because its tumors lack receptors for estrogen and progesterone as well as the HER-2 protein, which means women with triple negative breast cancer cannot benefit from two kinds of treatment that have transformed other breast cancer care: hormonal therapies and drugs that target HER-2.
So Houston Methodist researchers tried targeting the iNOS pathway with L-NMMA. The body produces nitric oxide naturally for normal health, but in triple negative breast cancer, increased nitric oxide signaling is linked to a poorer prognosis, the Houston Methodist team research showed.
Patients who received the combination therapy had an overall response rate of nearly 50%, compared to the usual 25% to 30% in patients with the same stage of disease and who receive standard treatment.
The team's non-randomized, non-blinded phase I/II trial involved a total of 35 triple negative breast cancer patients, 11 with locally advanced disease and 24 with metastatic disease. Most of the patients had already failed to respond to multiple chemotherapy regimens.
Patients received a maximum of six (21-day) cycles of the combination. L-NMMA was administered as a 2-hour intravenous infusion on days 1 to 5 of each cycle.
As many as 80% of participants with locally advanced tumors in the breast and 15% of those whose tumors had spread to other parts of the body responded to the combined treatment.
Next step: multinational phase III trials
Any side effects from the treatment — in each case a result of the docetaxel, not the L-NMMA — were minor and quickly resolved, according to Dr. Chang.
L-NMMA was initially developed for the management of cardiogenic shock — a phase III trial investigating such use found it was safe but of no benefit — before Dr. Chang's team tried it on cancer. She made a deal to secure the drug from a Cornell University pharmacologist who led the trial and still had vast supplies.
The next step for Dr. Chang and the team are multinational phase III trials to evaluate the L-NMMA and chemotherapy combination in a significantly larger number of TNBC patients. If those trials show positive results, the team plans to file for FDA approval of L-NMMA.
In addition, Houston Methodist plans to seek an orphan indication from the FDA for metaplastic breast cancer, an aggressive subtype of TNBC that accounts for less than 1% of all breast cancers. The National Cancer Institute has awarded Houston Methodist a grant to take the therapy into global phase III clinical trials, which will begin in late 2022.
Dr. Chang also said she plans to research the combination of L-NMMA and checkpoint blockade immunotherapy against triple negative breast cancer. Such immunotherapy has revolutionized treatment of many cancers, but by itself has only shown modest benefits against TNBC.
The Houston Methodist TNBC research has been supported by the National Cancer Institute, the Breast Cancer Research Foundation, the Moran Foundation, Causes for a Cure, the Center for Drug Repositioning and Development Program, and Dr. Mary and Mr. Ron Neal.