Innovation Center Continues to Reshape the Future of Clinical Care
Aug. 27, 2021 - Eden McCleskeyApproximately one month before the COVID-19 pandemic began, the Houston Methodist Center for Innovation opened its first laboratory space for clinicians and developers to test new technologies.
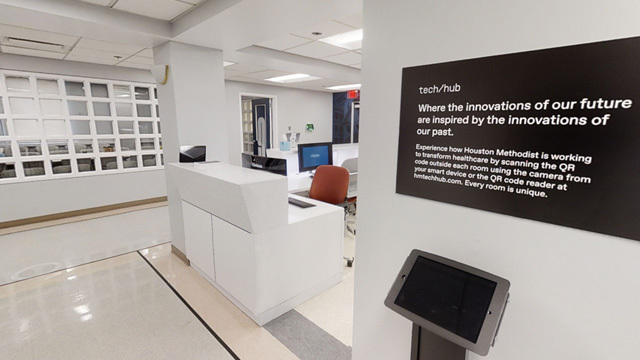
The Technology Hub, a renovated 3,500-square-foot wing of Houston Methodist's flagship Texas Medical Center location, was designed to showcase new digital health technology such as virtual reality, voice-controlled equipment and smart watch applications.
The idea, according to Roberta Schwartz, executive vice president and chief innovation officer, is to put hospitals in the driver's seat of the change occurring in the health care industry.
"We're either going to be disrupted or we're going to have to do the disruption ourselves," says Schwartz. "There's nobody who knows health care better than we do, so if we're going to transform the industry, I want that transformation to come from the inside."
In other words, be the Uber, not the cab company.
The timing of the Technology Hub's opening and the hospital's major investment in digital health couldn't have been better, given the arrival of the ultimate disrupter, COVID-19. The focus on reimagining the patient experience, enhancing access to care through digital platforms and creating nearly touchless clinical environments perfectly positioned the enterprise.
The focus is on solving unforeseen problems and refining digital health technologies that, for better or worse, recently underwent the biggest pilot test in history.
If telehealth appointments and iPad thermometers don't exactly seem cutting-edge anymore, remember this: "Innovation isn't always about the newest technology, it's about using existing technology better," says Josh Sol, administrative director of Houston Methodist Innovation and Ambulatory Clinical Systems. "What we talk about a lot is 'the art of the possible.' What can we leverage? What can we put forward — today or tomorrow, not a decade from now — to improve health care delivery and empower patients to feel more in control of their health?"
It's these type of achievable Research & Development projects the Center for Innovation is focused on. Here's the latest on four of the center's major efforts:
Clinical voice technology: Turning ambient listening into actionable intelligence
Houston Methodist is bringing voice technology and natural language processing into exam rooms, patient beds and ORs in hopes of improving the patient experience and decreasing physicians' reliance on distracting note-taking recorders.
A clinical pilot project kicked off several weeks ago to determine which technologies and interfaces — such as wall screens and different types of speakers — work best for patients and clinicians.
A similar pilot program for the OR will begin this fall. Through a unique collaboration with Amazon Web Services (AWS), Houston Methodist is the first hospital to ever pilot this type of technology in the OR.
Both projects are exploring how to integrate voice and transcription technologies with Epic and the International Classification of Diseases, effectively turning the conversation into medical code in real time. (Think: seeing your order pop up on a plasma screen at the drive-through and knowing it's correct before you move forward.)
The benefit: quickly converting time-consuming, labor-intensive and often inefficient tasks and functions into actionable items.
In the OR, for instance, a surgeon will be able to search or notate a patient's electronic health record or CAT scans using just his or her voice, rather than potentially corrupting the sterile environment touching a keyboard or mouse.
Intelligent automation: Syllable voice/chat bots handle heavy COVID-19 lifts
In 2020-21, the Houston Methodist call center and website experienced heavy spikes due to the demands of triaging patients, scheduling COVID-19 tests, coordinating convalescent plasma donations and, eventually, distributing COVID-19 vaccines.
The hospital system needed a solution that could allow it to handle the onslaught without burdening already strained operations. Rapidly expanding the number of full-time employees in existing call centers by 300%-400% would be unrealistic and cost prohibitive, and outsourcing to an external call center risked a loss of control.
Fortunately, the center had already been in talks to partner with Syllable, an AI system for managing phone calls and web chats, even before the pandemic hit. The partnership went live in May 2020, and since then Syllable has handled more than 90% of the hospital system's COVID-19 related interactions.
In one eight-day period, from December 29, 2020-January 5, 2021, the COVID-19 vaccine hotline fielded nearly 60,000 calls and over 25,000 text messages and added nearly 10,000 callers to the vaccine wait list, all by automation. By June 2021, the voice assistant had answered half a million calls and triaged almost 250,000 eligible patients to scheduling options, helping Houston Methodist deliver over 750,000-19 COVID-19 vaccines, more than any other hospital system in the state.
"This technology has worked so well, we've recently expanded the scope of work to support non-COVID calls and tasks," says Schwartz. "The best part is that we can dynamically scale up or down to accommodate fluctuations and answer every call without impacting our usual operations."
CareSense mobile platform guides patients through complex surgical pathways
Surgery can be overwhelming, not least because of the amount of information patients need to prepare for and recover from the procedure.
Yet patient understanding and adherence to pre- and post-operative guidelines is critical for surgical success; noncompliance can lead to cancellations, complications and readmissions. When Houston Methodist surgical teams sought to improve patient education, preparation and guideline adherence, the Center for Innovation partnered with CareSense to come up with a platform delivered by digital communication.
Under the partnership, Houston Methodist has reduced readmissions in most cases by 50% and length of stay by 25%. This also helped to conserve staffing needs as COVID-19 increased demands.
The platform allows patients to choose their preferred method of communication — emails, phone calls or texts — to receive information about their surgery. The messaging is broken into bite-size chunks that are easily understandable and actionable by individuals.
Rather than loading up patients with information at preoperative appointments, or at discharge, information is delivered at the most relevant time.
Clear and consistent patient communication helps patients feel confident in their recovery and comply with their surgeon's orders — without having to call the office and speak with a nurse. It also helps patients identify potential infections or other serious issues sooner.
The program, which has enrolled more than 4,000 patients, has produced some impressive numbers: 98% patient satisfaction, 80% patient engagement, a 50% reduction in readmissions, a 25% reduction in the length of stays, a 40% reduction in emails and calls, and a 10%-15% improvement in Hospital Consumer Assessment of Healthcare Providers and Systems survey scores.
Next steps include rolling out CareSense to an expanded number of service lines and hospital locations and integrating the platform into Epic. The continuum between the patient record and communications, say officials, offers greater opportunities to provide seamless patient experiences, enhance efficiencies, eliminate redundancies and, ultimately, improve outcomes.
Virtual ICU uses remote monitoring and predictive analytics to identify critical risks
The Virtual ICU (vICU) provides continuous intensivist coverage for Houston Methodist's more than 300 ICU beds. The vICU is a remote monitoring center that captures real-time physiological data and uses predictive analytic tools to rapidly identify critical risk factors and anticipate patient decompensation.
The vICU Operations Center is staffed by intensivists and critical care nurses who provide patient care by initiating earlier interventions and offering additional support to bedside ICU teams.
Patient rooms are equipped with high-resolution cameras and television monitors to allow for unobtrusive observation or consultations with the patient.
Since launching the pilot, program highlights have included:
- the installation of cameras and monitors in all 163 ICU rooms at Houston Methodist Hospital in the Texas Medical Center.
- the launch of 126 ICU beds — neurosurgical, medical, cardiac and cardiovascular — all within 10 days.
- 24/7 staffing that provides additional support to all bedside teams, an expansion of the original intent to focus on nighttime coverage. Such staffing also helps connect families with their loved ones during limited visitation due to COVID-19.
- responses to as many as 70 events per night (respiratory, cardiac, blood pressure, code blue, neurological, lab assistance, etc.).
- the admittance of as many as 20 patients by virtual MDs per night.
- as many as 100 team communications per night (bedside imaging, lab requests, MD services, handoffs, regular patient checks).
- the vICU responding to 3,500 alerts and caring for 15,000 ICU patients in 2020.